Background: Community acquired pneumonia (CAP) is one of the leading causes of hospitalization in the United States.[1] In an effort to improve the quality of care for this resource-intensive disease, our institution implemented a clinical decision support (CDS) pathway for CAP comprised of three phases: (1) education on best practices, (2) education and a CDS pathway coupled with active antimicrobial stewardship and provider feedback, and (3) education and CDS pathway without active stewardship. The final phase was completed on September 30, 2018. Since then, the CDS pathway has remained active. Following phase 2 and 3, length of IV therapy decreased significantly.[2] Antibiotic use at discharge, however, has not been evaluated since the end of phase 3. Thus, we aimed to characterize the sustained effect of the CDS pathway initiative on antibiotic overuse at discharge at our institution.
Methods: We conducted a retrospective cohort study of adult patients discharged from our tertiary care center with CAP between August 1, 2019 (ten months following completion of the inpatient CDS initiative) and January 31, 2020. Patients with complicating factors such as bacteremia, empyema, and deep-seeded infection were excluded. The primary outcome was antibiotic overuse at discharge,[3] defined using a previously published definition as unnecessary antibiotic use (patient not meeting diagnostic criteria for pneumonia), excess duration, or suboptimal fluoroquinolone use at discharge. Secondary outcomes were length of stay, 30-day readmission, emergency department visit, and mortality.
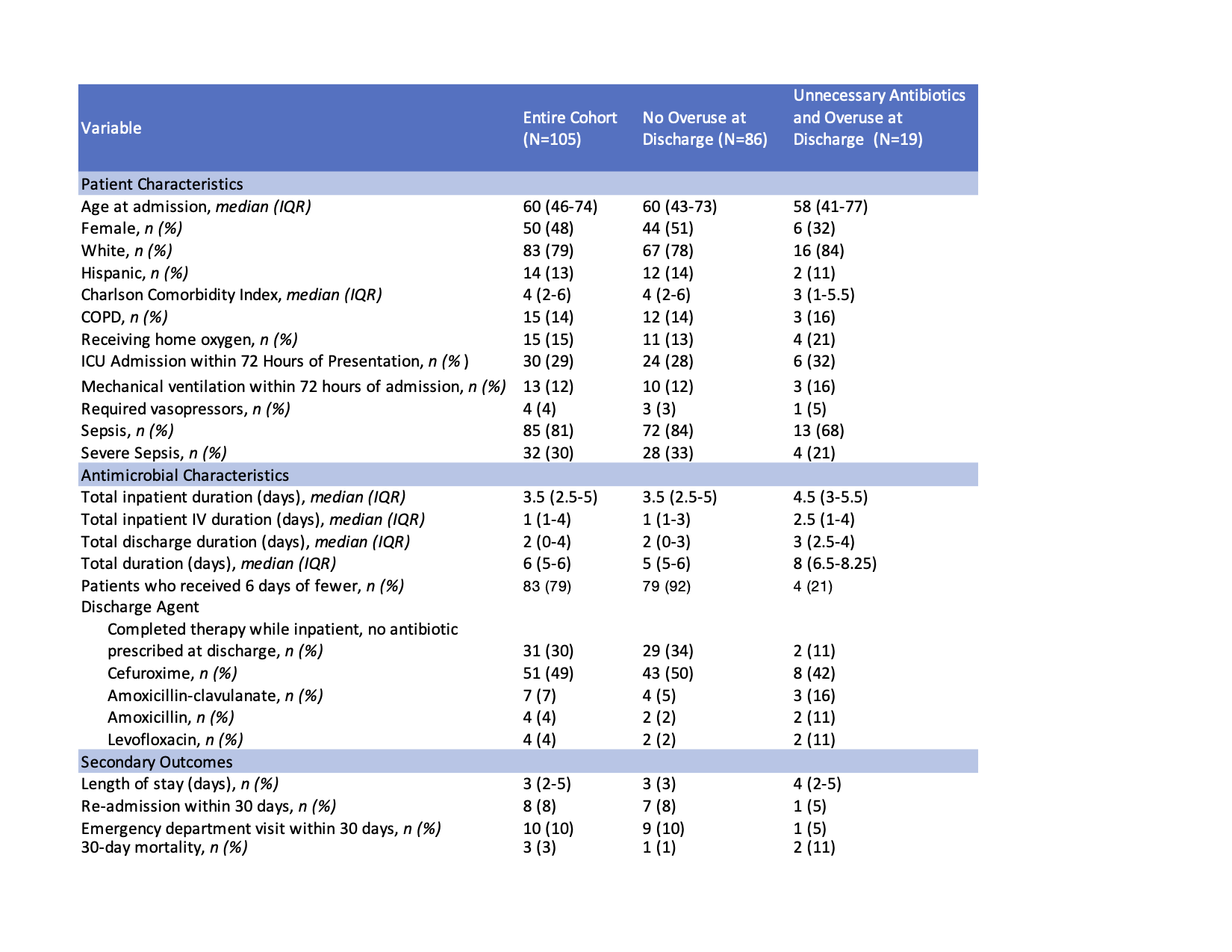
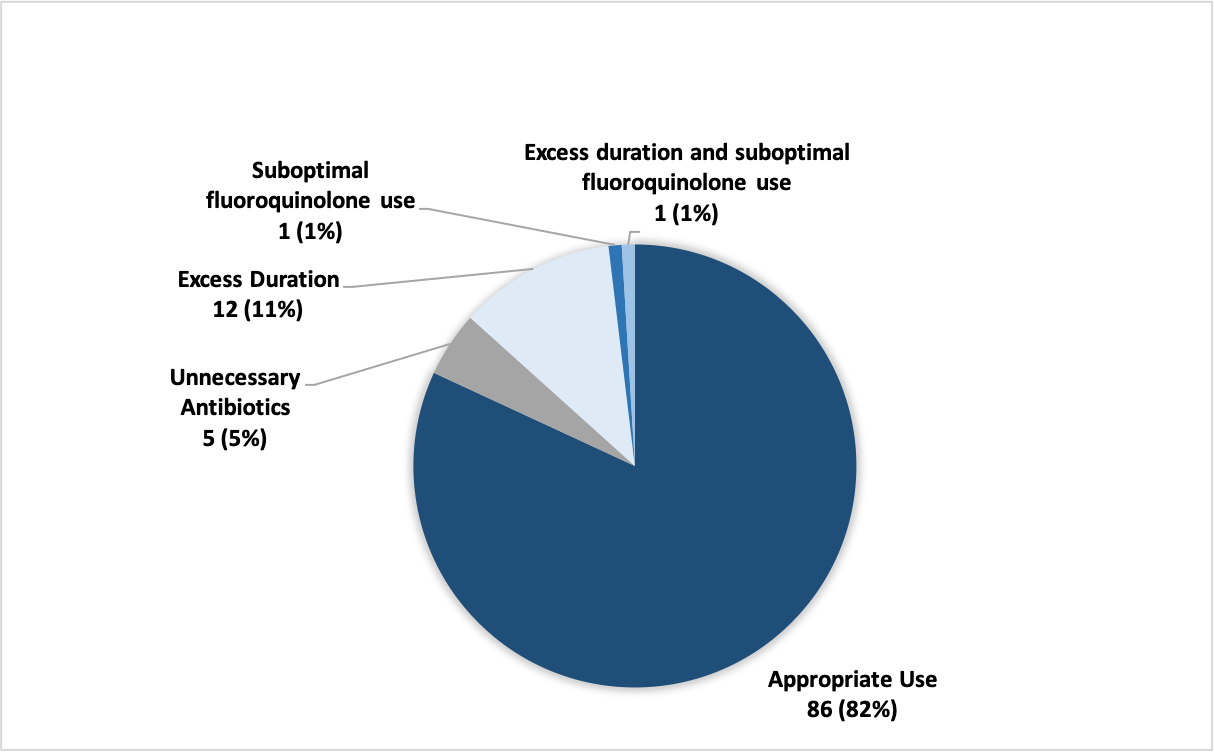
Results: Of 126 patient reviewed, 105 without complicating factors were eligible for inclusion. The median age was 60 and the median Charlson Comorbidity Index was 4 (Table 1). Thirty patients (29%) had an ICU admission within 72 hours of hospitalization. Median antibiotic duration was 6 days (IQR 5-6 days), with 83 (79%) of patients receiving a total duration of six days or fewer. Thirty-one patients (30%) completed antimicrobial therapy while inpatient and had no antibiotic prescribed at discharge. Fifty-one patients (49%) were discharged with cefuroxime; only 4 patients (4%) were discharged with a fluoroquinolone. In total, 18% (19/105) of patients had antibiotic overuse at discharge: antibiotics were deemed unnecessary in 5 (5%) of cases, 12 (11%) were found to have excess duration, one (1%) had suboptimal use of a fluoroquinolone, and one (1%) had both excess duration and suboptimal fluoroquinolone use (Figure 1). Eight patients (8%) were readmitted in 30 days and the median length of stay was 3 days (Table 1).
Conclusions: At our institution, antibiotic overuse at discharge was lower than antibiotic overuse in prior studies.[3] Specifically, the majority of patients hospitalized for CAP received six days of antibiotic therapy or less and most patients were discharged with cefuroxime. These results imply a sustained and lasting effect of our institution’s CAP CDS pathway (which included an antibiotic stop date and early transition to cefuroxime) coupled with prospective antimicrobial stewardship review on reducing antibiotic overuse, particularly during care transitions, while maintaining good patient outcomes. The CAP pathway intervention represents an opportunity to sustainably expand antibiotic stewardship at discharge, potentially across hospitals.