Background: Since 2020, UNC Hospitals has increasing numbers of patients who no longer require acute level of care. A portion of these patients have longer length of stay exceeding 30 days while awaiting disposition. This is noticeable in our percentage of long length of stay patients hospitalized 31-60 days (6.8% in 2022 vs 6.0% in 2020) and >60 days (8.1% in 2022 vs 5.2% in 2020). There is a growing body of literature focused on patients who are medically ready for discharge from the hospital, but who experience significant discharge barriers.1,2,3 A recent study published in 2023 by Bann et al. reviewed patients medically ready for discharge at 15 academic medical centers. They found 44% of patients with major discharge barriers spent a month or longer awaiting discharge from the hospital while medically ready, extending length of stay and unnecessarily utilizing hospital resources when patients are appropriate for a lower level of care.1
Purpose: Our physician advisor team identified predominant barriers associated with discharge delays related to prolonged hospitalizations.
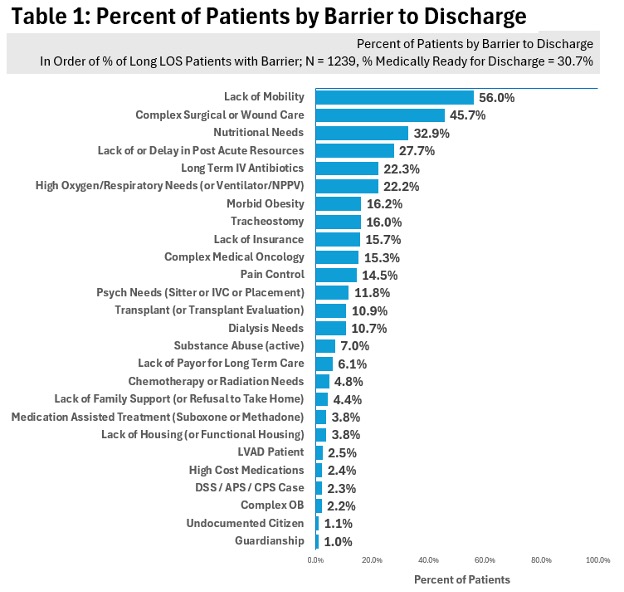
Description: During a one-year period from May 2023 until May 2024, hospitalized patients with a prolonged length of stay at UNC Hospitals were reviewed in depth on hospital day 20 to determine potential discharge barriers. Our physician advisor team reviewed these encounters and identified 26 distinct discharge barriers (listed in Table 1) associated with prolonged hospitalization. We also identified and labeled patients with a unique treatment team to track those who were medically ready for discharge. Pediatric patients were excluded from this cohort.
Conclusions: A total of 1,239 unique patient encounters were reviewed over one year. Lack of mobility was the leading discharge barrier, affecting 56% of all patients in the cohort (Table 1), and specifically 72.9% of patients medically ready for discharge (Table 2). Given the prolonged hospitalization of many patients accumulating medically unnecessary days, addressing functional mobility deficits as a discharge barrier for our patients became of high importance, requiring immediate resources allocation. For those patients who were medically ready for discharge, Lack of or Delay in Post-Acute Resources was the second most frequent barrier, affecting 56.1% of patients. This data is supported by prior studies identifying post-acute resources as a significant barrier prolonging hospital stays.1,2,3 Complex Surgical Wound Care and Nutritional Needs were the second (45.7%) and third (32.9%) leading discharge barriers associated with prolonged hospitalizations. Our surgical and medical teams take care of many patients with complex wounds that poorly heal due to a multitude of factors. Need for more coordinated nutritional support has been shown to be one of these factors necessary for appropriate wound healing,5,6 resulting in additional resources to coordinate this care in the inpatient and outpatient settings.Our manual chart review has led to the development of an automated process within the electronic medical record (EMR) to identify these discharge barriers in real time. A dashboard will display both historical and daily discharge barriers for individual patient encounters with prolonged hospitalizations. Next steps in this work include operationalizing this dashboard across the health care system and creating an algorithm augmented by Natural Language Processing (NLP) to be implemented in our EMR.