Background: Many institutions rely on informal training for internal medicine (IM) residents about how to provide effective discharge communication to patients and their caregivers. Complete instructions are essential to safe transitions of care. At our institution, we evaluated baseline knowledge of these topics among IM residents, and assessed how an educational module impacted residents’ knowledge, attitudes, and self-assessed skills preparing discharge communication.
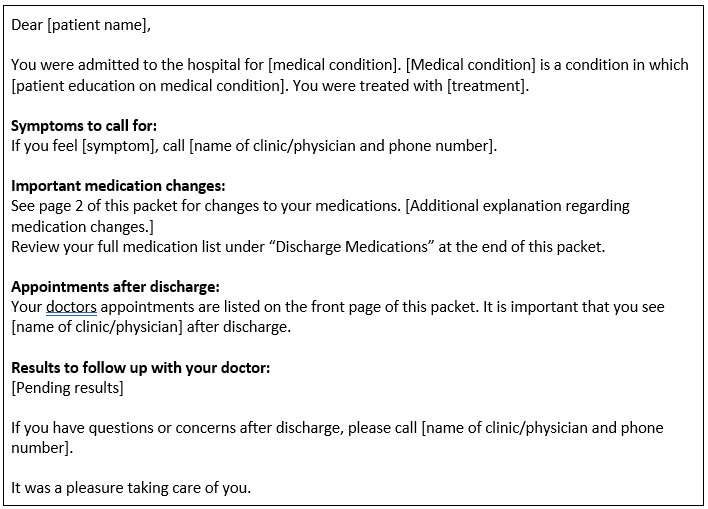
Methods: To assess baseline attitudes among senior IM residents, PGY2 and PGY3 residents who had not received formal discharge communication education were given a survey about optimal patient discharge education. Separately, an educational module on discharge communication was built for PGY1 residents. Content was developed based on best practices in the literature. A template for written patient discharge communication was developed (Figure 1)1-3. The one-hour module was delivered in a one-hour didactic. Attendees received pre-/post-session surveys to assess changes in knowledge, attitudes, and self-assessed skills. To compare pre- and post-test averages, t-tests were used to determine statistical significance.
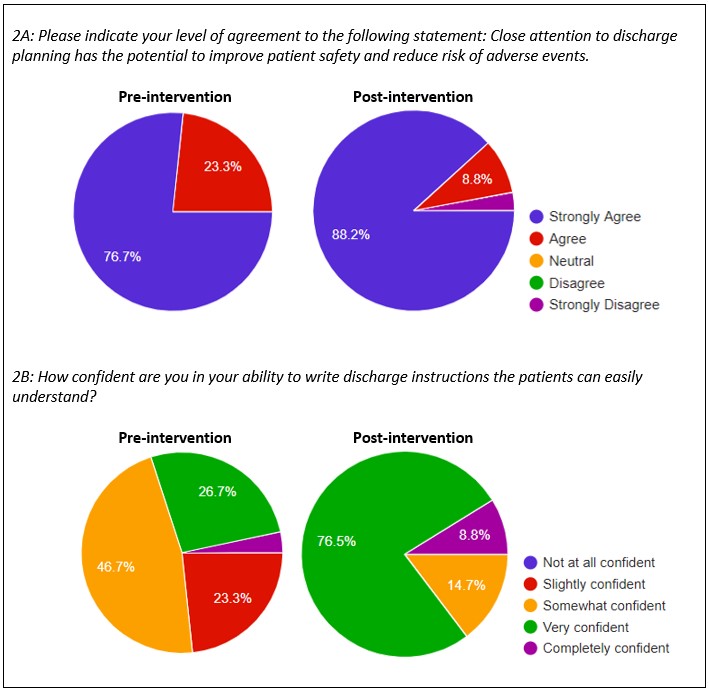
Results: 31/89 (34%) PGY2/PGY3 residents responded to the needs assessment survey. The majority of residents reported “sometimes” writing discharge communication, while only 29% “always” provided written discharge communication. Topics included in written discharge communication included medication changes (83.4%), future appointments (73.3%), education about the hospitalization (43%), and anticipatory guidance (33.3%). Few residents included the hospital primary diagnosis (23.3%) or pending results (6.7%). Reported barriers to writing discharge communication included lack of time and being unaware of where/how to document. The majority (74.1%) of residents did not report feeling “very confident” preparing written discharge communication.Of 46 PGY1s, 34 received the discharge communication curriculum, with another 12 planned to do so. Of these, 30 (88.2%) completed the pre-session survey and 34 (100%) completed the post-session survey. Prior to the didactic, 93.3% felt they had not received enough formal training on discharge communication and 96.7% desired more formal education. Pre-intervention, 76.7% strongly agreed that discharge planning can improve patient safety compared to 88.2% post-intervention (p=0.11) (Figure 2A). Only 26.7% reported feeling “very confident” in their ability to write discharge instructions pre-session, while 73.5% reported feeling “very confident” post-session (an increase of 46.8%, p < 0.001) (Figure 2B).
Conclusions: Residents at our institution inconsistently provide written discharge communication to patients. Many reported a lack of confidence performing this skill. A discharge communication curriculum led to increased confidence in communicating discharge plans to patients and enhanced recognition of the importance of discharge communication in patient education and safety at the transition of care. One limitation of these results is that data is self-reported without direct assessment of residents’ skills or behaviors; future interventions will evaluate whether discharge communication education for residents and the use of a standardized template changes behavior and frequency of completing written discharge communication.