Background: There are no guidelines for designing or evaluating fixed-content signs or electronic displays used to communicate patient-related information in hospital rooms. Accordingly, there is the potential for the displayed information to be ignored, misinterpreted, or distracting in the complex hospital room environment where patients, nurses, and physicians change frequently.
Purpose: To address this shortcoming, we developed a new guideline employing human factors expertise to inform the development of signs and other displays for communicating medical information to healthcare workers in hospital rooms. This guideline was then applied and refined to support the development of a new electronic bedside display for improving physician awareness during rounds of common hazards hidden under the sheets – catheters and wounds.
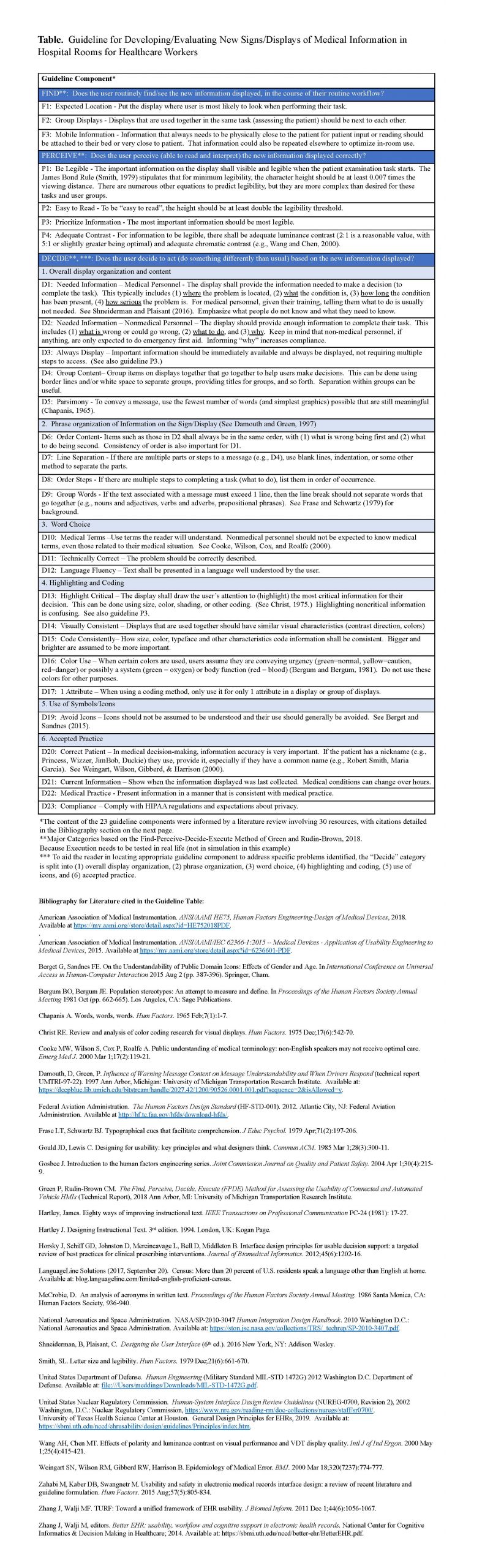
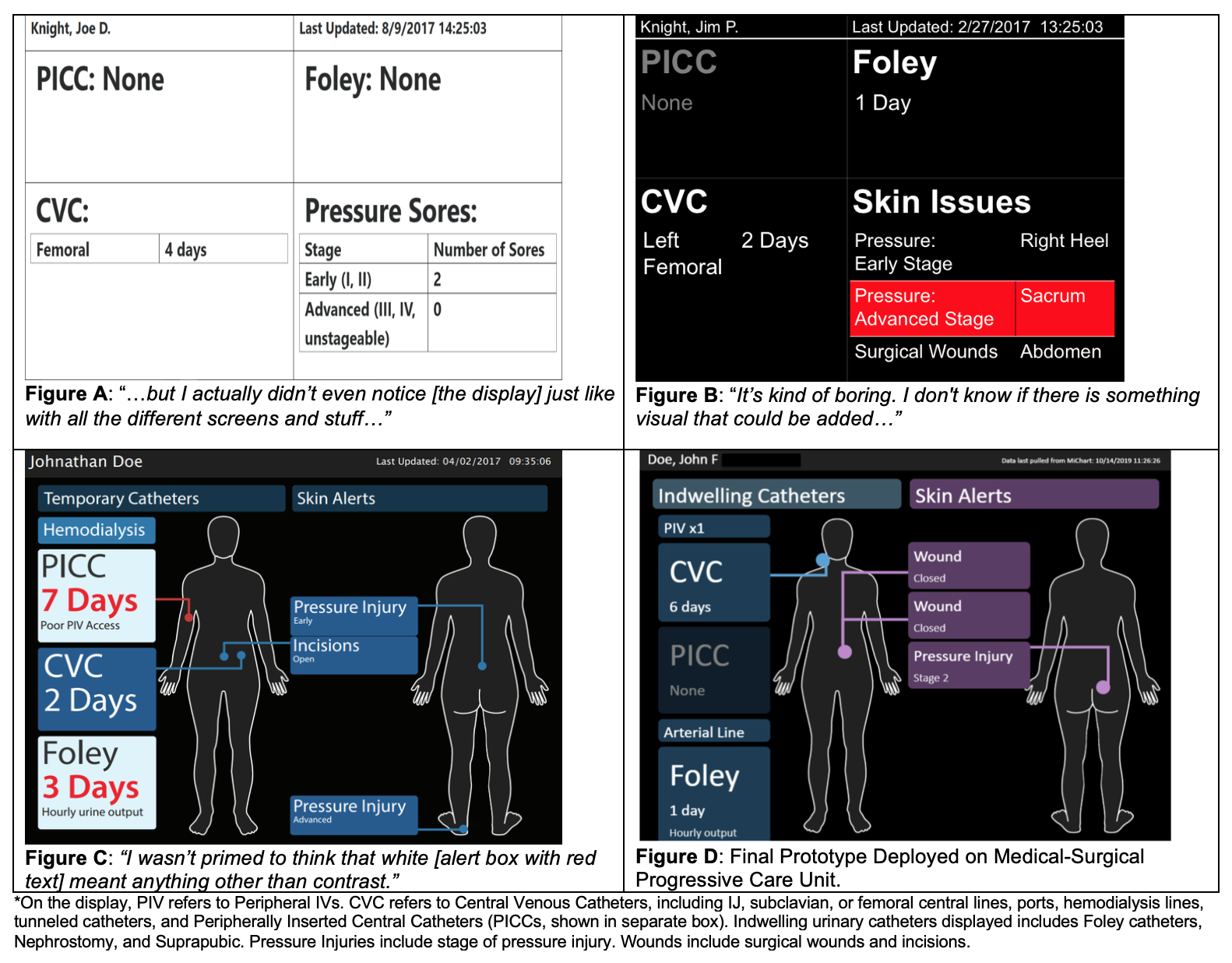
Description: Guideline development began with physicians using prototypes of displays showing catheter and wound data in a simulated hospital room with a manikin patient. The displays evolved based on the physicians’ feedback. Of interest were how the use of the display coincided with usual workflow, the tasks the display could support, and the types of problems that occurred with use of each iteration of the display. The problems were revealed by observing 12 physicians ‘think aloud’ about their differential diagnosis as they performed a history and patient examination while rounding on 2 simulated patients experiencing a fever as a new condition. Observations were performed and analyzed by a hospitalist with expertise in patient safety, a human factors expert, and a project manager experienced in qualitative data methods who introduced the clinical scenario simulations and performed post-simulation debriefing. The Find-Perceive-Decide-Execute (FPDE) Method was applied. The FPDE considers the four steps involved with utilizing information on a display, and the failures that can occur at each step. The FPDE Method provided a basis for making decisions about the overall organization of the display, what data needed to be included, the size and color of text, the words used, and other matters relating to content. A narrative review of 30 literature sources informed the individual components of the guideline. The guideline developed for designing and evaluating new signs and electronic displays in hospital rooms is summarized in the Table. The Figure illustrates the major changes made in the prototype informed by the guideline and simulation participants for the display of catheter and wound information to healthcare workers, as well as the final prototype that was recently deployed in a 20 bed Medical-Surgical Progressive Care Unit.
Conclusions: This project produced 1) a new guideline for applying human factors expertise to develop and evaluate new signs and electronic displays for medical information in the hospital room environment, applicable for low tech (paper signs) and high tech applications, and 2) a prototype for displaying urinary and vascular catheter information (presence, location, and duration of use) as well as wounds (presence, type, location, and severity if pressure injury).