Case Presentation:
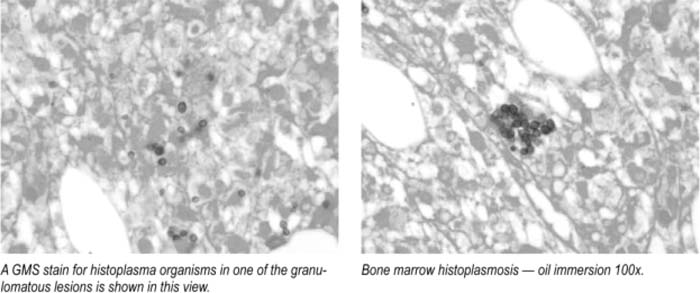
A 54‐year‐old woman with no past medical history presented with a 2‐month history of increasing fatigue, fever, and loss of appetite. She denied any other symptoms. She was pale and febrile (101.7°F) and had ecchymosis over her arms, but the physical exam was otherwise normal. Labs revealed Hb 8.3, WBC 0.65 with 76% neutrophils and 21% lymphocytes, platelets 23 K, Alk Phos 228,1 bili 1.8, AST 94, ALT 96. CTof the chesl and abdomen revealed mediastinal adenopathy and splenomegaly of 15.5 cm. BM biopsy showed small budding yeast forms suggestive of histoplasma capsulatum and no evidence of malignancy or myelodysplastic syndrome. Urine histoplasma Ag was strongly positive. Immunodeficiency panel revealed a CD4 count of 3. An extensive autoimmune and other infectious workup including HIV and HTLV was negative. The pancytopenia, splenomegaly, and abnormal liver enzymes were thought to be secondary to disseminated histoplasmosis. However it was not clear if The disseminated infection was a consequence of prolonged immune suppression (idiopathic CD4 lymphocytopenia) or a cause of CD4 lymphopenia. The patient responded to IV amphotericin and was discharged on itraconazole with a plan to follow CD4 counls in 2 months.
Discussion:
Disseminated histoplasmosis is a progressive extrapulmonary infection presenting with fever, fatigue, and weight loss or symptoms pointing to oropharynx, Gl, CNS, and adrenal involvement. Differential diagnosis includes malignancy, infection, or inflammatory disease (IBD, sarcoidosis). Urine antigen is the most sensitive rapid assay. Ab serology is negative in the immunosuppressed. Blood cultures are positive in 50% and BM cultures in 75% of patients with pancytopenia. Severe disease is treated with liposomal amphotericin B for 1–2 weeks, followed by itraconazole to complete at least 1 year ol therapy. Itraconazole is the initial therapy for mild to moderale symptoms. Most patients are immunosuppressed or extremes of age. Chronic progressive dissemination occurs rarely in older adults with no known immunosuppression from unidentified defects in cellular immunity. Idiopathic CD4 lymphocytopenia (ICL) is defined by persistent CD4+ T‐cell lymphopenia in the absence of infection with HIV‐1 or any other cause of immunodeficiency. CD4 counts should be < 300 or < 20% of total lymphocytes on 2 separate analyses. Many serious infections such as bacterial sepsis or measles can lead to transient CD4 lymphopenia from consumption of cells. Differentiating between ICL as a cause of infection and infection as a cause of profound CD4 lymphopenia can be challenging because in most cases T‐cell subsets are not evaluated until the patient becomes overtly ill, and il is impossible to say which condition was present first.
Conclusions:
Hospitaiists should be aware of (1) disseminated histoplasmosis as a rare cause of pancytopenia due to marrow infiltration as it has good prognosis with treatment, and (2) ICL, a rare immunodeficiency, as it is responsible for opportunistic infections in HIV‐negalive patients, and they need primary prophylaxis similar to AIDS patients
Author Disclosure:
R. Bahuva, none; W. Morris, none; M. Patel, none; S. Kandpal, none.