Background:
Growing use of peripherally inserted central catheters (PICCs) has led to the development of certification programs for PICC operators. Much like the debate regarding certification in medicine, whether such certification influences clinical care is unknown. This knowledge gap is relevant for health systems that hire operators based on certification status and for hospitalists who work closely with these providers in securing venous access. Therefore, we conducted a national survey to compare practices between certified and uncertified vascular access providers.
Methods:
A web-based survey was distributed through the listservs of two vascular access societies, with a combined estimated membership of 8385 (of which an estimated 5662 are PICC operators). Questions regarding experience, practice, and knowledge related to PICC insertion and care were posed. Bivariate comparisons between certified and non-certified practitioners were conducted using chi-square, Fisher’s exact, or t-tests, as appropriate.
Results:
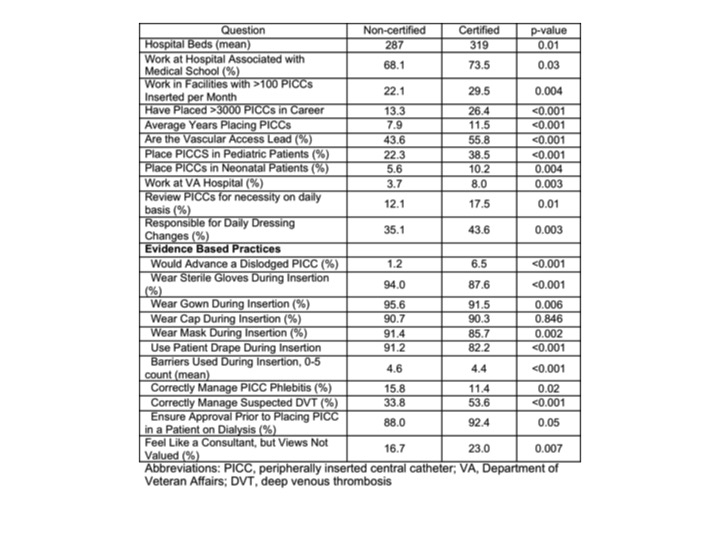
Of the 2762 potential respondents who accessed the survey, 1698 (61.5%) were deemed eligible and completed the survey. Those who did not place PICCS or had taken the survey previously were excluded. Of the 1450 respondents who provided certification status, 1020 (70.3%) stated they held a vascular-access certification. Roles and settings in which certified and non-certified providers practiced varied considerably (Table). Compared to non-certified operators, certified operators had more years of experience placing PICCs (p<0.001), had placed more PICCs (p<0.001), and were more likely to be the vascular access lead for their organization (p<0.001). Self-reported adherence to evidence based practices was variable (Table). Certified operators were more likely to report they re-advanced dislodged devices (p<0.001) and did not follow certain sterile insertion practices. However, compared to non-certified operators, they were more likely to report the correct management of suspected PICC-related deep venous thrombosis (p<0.001). Notably, certified operators were also more likely to view themselves as consultants whose views were not valued by members of the team (p=0.007).
Conclusions:
Important differences between certified and non-certified vascular access operators exist. Nonetheless, reported variability in the use of evidence-based practices among those certified suggests that future studies to evaluate sources of such variation may be necessary. Given the ongoing debate regarding the role of certification in other fields, understanding the impact of vascular access certification on care and outcomes in hospitalized patients may prove useful.