Background: The position of the tip of a peripherally inserted central catheter (PICC) is associated with deep vein thrombosis (DVT). Optimal position of the tip is the cavoatrial junction; more proximal tip positions are associated with greater risk of DVT. EKG-guidance has recently emerged as a modality to ensure proper tip position. Compared to chest X-rays, EKG-guidance is quicker, can be performed at the bedside and is thought to be more physiologic as it locates to the SA node in the cavoatrial junction. However, whether or not EKG-guidance is associated with a reduction in PICC-DVT is not known.
Methods: We used data from the Michigan Hospital Medicine Safety (HMS) Consortium, a 47-member Blue Cross Blue Shield-of Michigan funded collaborative to examine risk of DVT following EKG-guided placement. Trained abstractors collect standardized data from medical records at each site. An upper extremity ultrasound showing thrombus was used to define PICC-DVT. Generalized estimating equations (GEE) were used to assess risk of DVT between EKG vs. non-EKG guided PICC placement, with adjustment for patient-, device- and hospital-level factors.
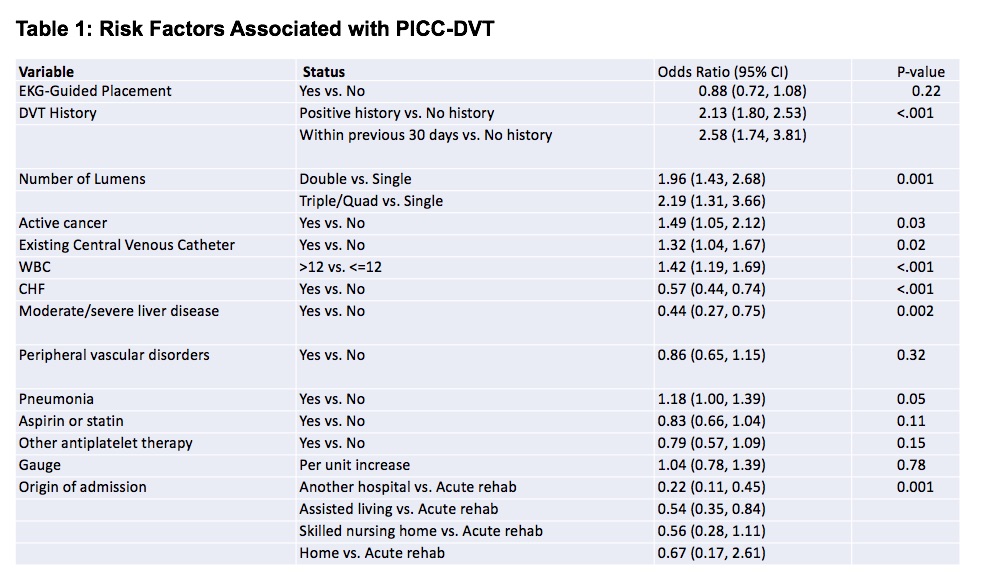
Results: A total of 23,828 patients were included in the analysis: 10,267 underwent EKG-guided PICC insertion while 13,561 did not. No differences in gender, race, Charlson comorbidity index or cancer history were observed between both groups. However, those undergoing EKG guidance were more likely to have moderate or severe liver disease (OR=1.12, 95%CI=1.01-1.24) but less likely to have CHF (OR=0.74, 95%CI=0.89-0.95), peripheral vascular disorders (OR=0.89, 95%CI=0.82-0.95), pneumonia (OR=0.93, 95%CI=0.88-0.98), or take an aspirin or statin (OR=0.88, 95%CI=0.83-0.92). PICCs placed using EKG guidance were less likely to be single lumen (OR=0.89, 95%CI=0.83-0.96 for double lumen and OR=0.82, 95% CI=0.71, 0.94 for triple lumen devices). Multivariable GEE models found no statistically significant association between EKG guidance and risk of DVT (OR=0.88, 95%CI=0.72-1.08). Factors most associated with PICC-DVT included DVT history within 30-days (OR=2.58, 95%CI=1.74-3.81), number of catheter lumens (OR=1.96, 95%CI=1.43-2.68 for double lumen and OR=2.19, 95% CI=1.31, 3.66 for triple lumen devices), and active cancer OR=1.49, 95% CI=1.05, 2.12).
Conclusions: EKG-guidance for PICC placement was not associated with reduction in DVT compared to non-EKG guided insertion in this large study. While placement using EKG facilitates insertion and verification of tip position at bedside, it may not reduce risk of thrombosis over conventional chest X-ray.