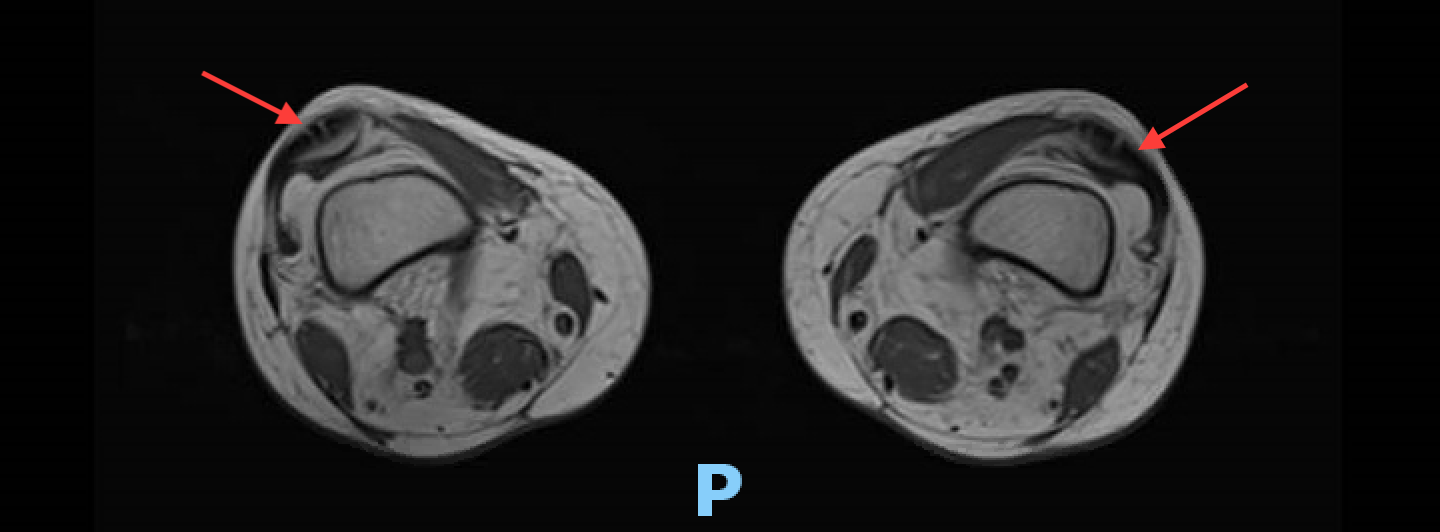
Case Presentation: A 60 year old man with a prior history of cutaneous sarcoidosis was admitted to the hospital with fatigue, myalgias, fever, and hypotension. His physical exam revealed a maculopapular erythematous rash on his trunk and bilateral lower extremities. Of note, three weeks prior to his presentation, he was treated with a ten day course of Clindamycin for presumed strep throat. His symptoms persisted, and he was then prescribed a five day course of Azithromycin for “walking pneumonia”. Initial labs were notable for mild transaminitis and a lactate of 5.4. In addition, he had a CK level as high as 5650 and eosinophilia as high as 19.2%. He underwent an infectious work up that was all negative and included a CT angiogram of the chest and abdomen/pelvis, viral panel, and blood and urine cultures. He was treated with norepinephrine and empiric vancomycin and piperacillin/tazobactam for possible toxic shock syndrome. Eventually, he improved and was discharged home. About a week after discharge, he was re-admitted to the hospital with the same presentation and a newly developing dysphagia. Again he required pressor support and was treated with broad spectrum antibiotics. This time his eosinophilia peaked to 31% and his CK level was greater than 50,000. He received an extensive infectious workup, rheumatologic/autoimmune work up, and evaluation for adrenal insufficiency, which were all unremarkable. He underwent an upper endoscopy with no identified cause for his dysphagia. Due to sinus bradycardia and his history of sarcoidosis, a cardiac MRI was obtained which was negative. A MRI of his femur, for his myalgias and CK level, was done which showed myositis. He was treated with high dose methylprednisolone then transitioned to oral prednisone. All of his symptoms resolved, and he was discharged on prednisone daily.
Discussion: Taking into account this patient’s clinical picture and extensive unremarkable work up, drug rash with eosinophilia and systemic systems (DRESS) likely went unnoticed. DRESS can occur anywhere from 2-8 weeks after the exposure to an offending agent. It is most commonly associated with anti-epileptic agents and antimicrobial agents, however, there is no comprehensive list of all known offending agents. In this scenario, the patient was exposed to azithromycin and clindamycin weeks prior to his initial presentation, both of which have been associated with DRESS in some literature. Interestingly, DRESS can have a relapsing form within days to weeks of the initial presentation despite cessation of the causative agent. This patient illustrated the key features of DRESS. Of note, the most common organ involved in DRESS is the liver. However, what was particularly profound was this patient’s rhabdomyolysis and muscle involvement. This is a rare finding that can be seen in DRESS. Unfortunately, no muscle biopsy was performed. A validated scoring system, the RegiSCAR criteria indicated that for this patient DRESS is a “probable diagnosis”.
Conclusions: Signs consistent with septic shock should be treated empirically given its high mortality rate. However, once infection has been ruled out, it is crucial to recognize that DRESS can present similarly to sepsis with a relapsing form that may go unnoticed due to the fact that it can occur despite cessation of the culprit agent. Additionally, even though it is rare, myositis can be one of the manifestations of DRESS. Ideally, a muscle biopsy would have solidified the diagnosis, but the RegiSCAR criteria can be utilized as a surrogate to guide management and treatment.