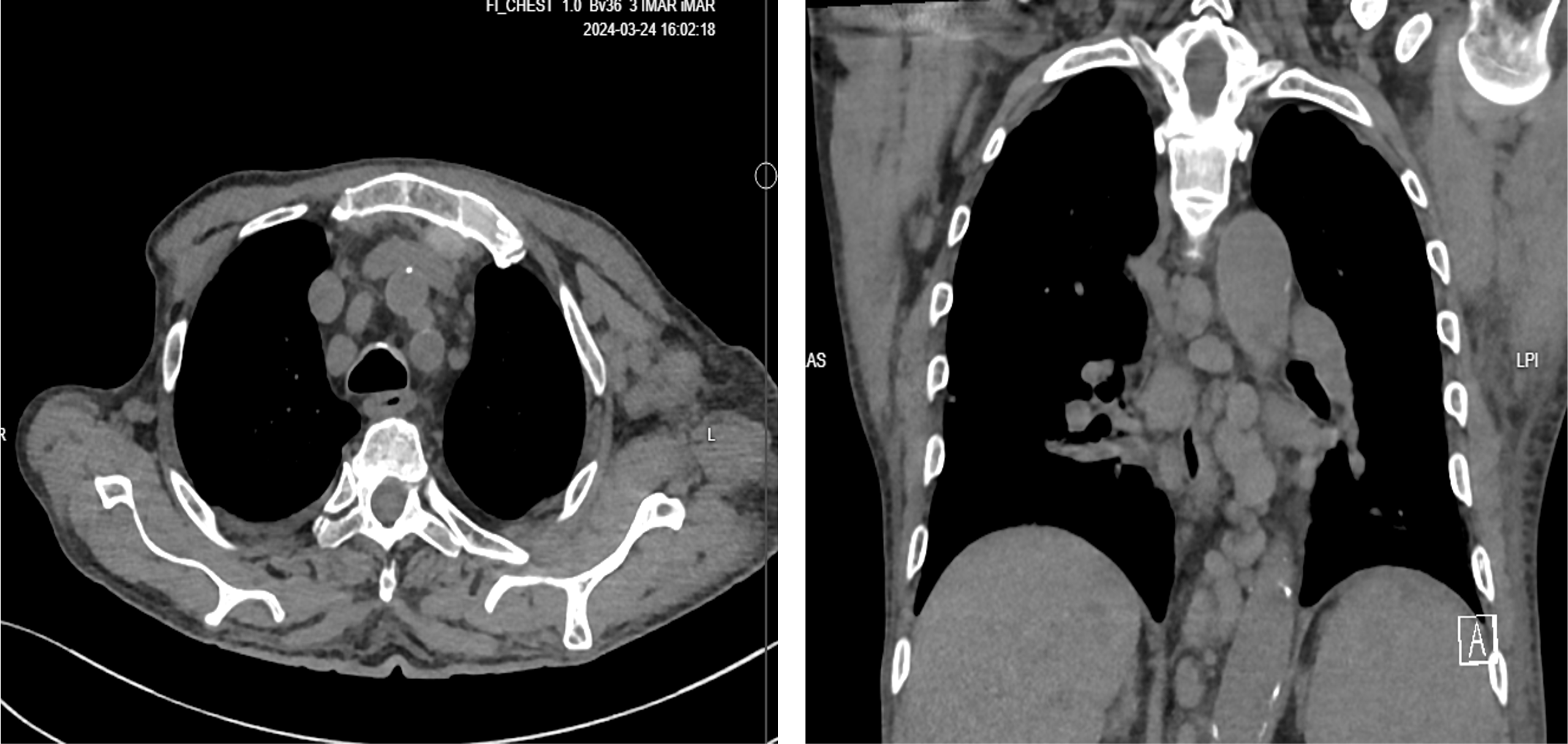
Case Presentation: Mycosis fungoides (MF) is a rare cutaneous T-cell lymphoma that progresses from patch-stage dermatitis to tumor-stage lesions. While primarily a dermatologic malignancy, MF can involve systemic organs or transform into more aggressive malignancies. Composite lymphomas (CL), characterized by the coexistence of two distinct lymphomas in one patient, are rare and diagnostically challenging. We present a rare case of a 73-year-old male with MF, managed with ultraviolet (UV) therapy, who developed left upper extremity swelling, low-grade fever, and leukocytosis. His white blood cell (WBC) count increased to 70,000/µL with predominantly neutrophilia, monocytosis, 15% lymphocytes, and 2.3% atypical cells. He exhibited tumor lysis syndrome (TLS) and acute kidney injury (AKI), requiring urgent hemodialysis. Laboratory findings showed elevated C-reactive protein (CRP) of 217 mg/L, lactate dehydrogenase (LDH) of 1774 U/L, and lactic acidosis (pH 7.27). A septic workup was positive for COVID-19, and computed tomography (CT) imaging demonstrated extensive lymphadenopathy and splenomegaly. Given his aggressive presentation, urgent peripheral blood flow cytometry initially suggested transformation to T-prolymphocytic leukemia. However, subsequent analysis confirmed high-grade B-cell lymphoma (B-LL), indicating a composite lymphoma. Although dose-adjusted EPOCH-R chemotherapy was planned, his rapid deterioration and progression to multi-organ failure delayed treatment.
Discussion: The coexistence of MF and B-LL is exceptionally rare, with few cases reported. Prognosis is poor due to the aggressive nature of both malignancies and their interplay. The pathophysiology of simultaneous MF and B-LL is unclear, but chronic immune dysregulation in MF may predispose patients to secondary hematological malignancies like B-LL. Dysregulation of both T-cell and B-cell pathways complicates treatment. Suspicion for dual malignancies should be raised in MF patients with atypical systemic symptoms, rapid leukocytosis, or metabolic derangements like TLS or lactic acidosis. Targeted therapies for high-grade B-cell lymphomas are challenging in composite lymphomas. Dysregulated T-cell and B-cell lines complicate B-cell-directed treatments, increasing the risk of immunosuppression or exacerbation of T-cell lymphoma. Early recognition and multidisciplinary intervention are essential, but achieving disease control remains difficult due to the aggressive nature of the malignancies and challenges in treating dual hematological involvement.
Conclusions: This case underscores the rarity of composite lymphomas involving T-cell (MF) and B-cell (B-LL) lineages, highlighting the need for early diagnosis and tailored management. Further research is needed to understand mechanisms and improve treatment strategies for these complex malignancies.