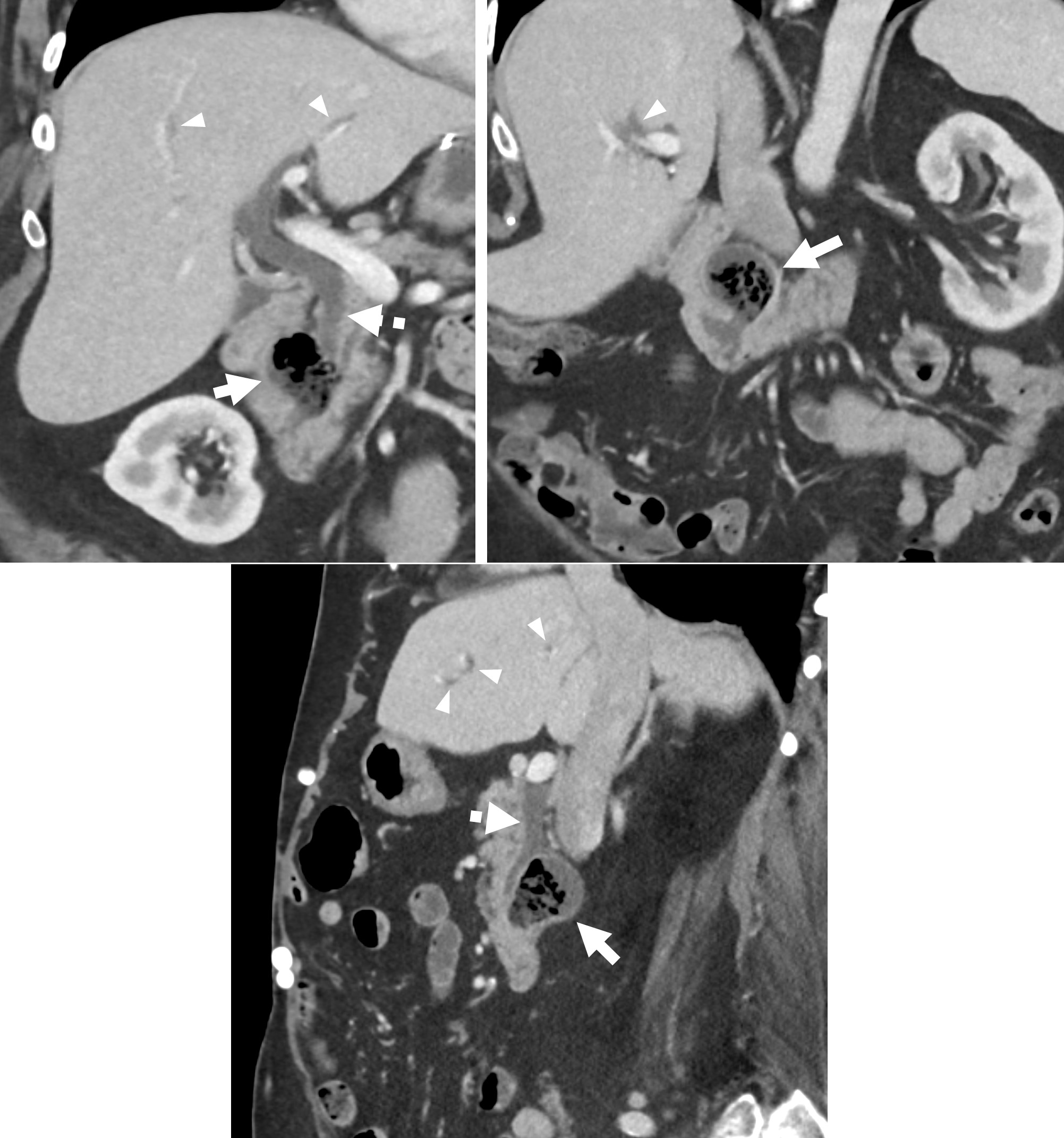
Case Presentation: A 74-year-old female with a history of sigmoid diverticulitis 9 months prior, C. difficile, gastroesophageal reflux disease, hypertension, coronary artery disease, and a surgical history of bariatric surgery, hernia repair, hysterectomy and appendectomy, presented to the emergency department for progressive epigastric, right upper quadrant (RUQ), left upper quadrant (LUQ), abdominal pain for 1 day. The pain was described as a discomfort that did not radiate to the back, shoulders or jaw and was not related to meals. She reported nausea, and recent loose stools which had resolved. She denied emesis, fever, chills, hematochezia, melena, hematemesis, dysuria, sick contacts, international travel, and changes to diet. She did not smoke or drink alcohol. She was afebrile (36.5℃), without tachycardia (65bpm), but was hypertensive (159/71 mmHg), mildly tachypneic (20) and with O2 saturation of 98%. She was not jaundiced on exam and without scleral icterus. On abdominal exam, there was pain on palpation of the epigastrium, as well as the RUQ and LUQ. There was no pain in the left lower quadrant. The abdomen was soft and nondistended without any peritoneal signs. Labs revealed a mild leukocytosis with a WBC count of 10.1. AST and alkaline phosphatase were slightly elevated at 67 and 144, respectively. ALT and total bilirubin were normal. EKG showed normal sinus rhythm and suggestions of left ventricular hypertrophy which was unchanged from previous. CT abdomen and pelvis was suggestive of a possible colovesicular fistula. Additionally, findings were suggestive of diverticulitis of a periampullary duodenal diverticulum with new mild dilation of the biliary tree which was to represent possible Lemmel syndrome (Figure 1). She was started on IV antibiotics and colorectal surgery was consulted regarding the colovesicular fistula. Surgery confirmed the diagnosis but recommended outpatient follow-up. She was discharged on an oral antibiotic regimen for small bowel diverticulitis.
Discussion: Non-Meckel’s small bowel diverticula are rare, with a reported prevalence of 0.5-1.9%, and most commonly affects the duodenum. While patients with small bowel diverticula are typically asymptomatic, and diagnosed incidentally, rarely complications can manifest in approximately 5% of those with duodenal diverticula including small bowel obstruction, diverticulitis, gastrointestinal bleeding. Periampullary duodenal diverticulitis is extremely rare and scarcely reported in the literature. A rare complication of periampullary duodenal diverticula/diverticulitis, as possibly seen in our patient, is Lemmel syndrome. Lemmel syndrome is an exceptionally rare condition where periampullary duodenal diverticula, and in our case, diverticulitis, leads to obstruction of the common bile duct (CBD) due to mass effect. While this condition classically presents with obstructive jaundice, this is not seen in all cases, similar to our patient. In our case, the duodenal diverticulitis was likely caught and managed early preventing significant obstruction of the CBD and cholestasis.
Conclusions: Here we present a rare case of periampullary duodenal diverticulitis possibly complicated by Lemmel syndrome presenting as non-specific abdominal pain which is scarcely reported in the literature. While rare, small bowel diverticulitis should be in the differential diagnosis for abdominal pain, especially if associated with suggestions of cholestasis.