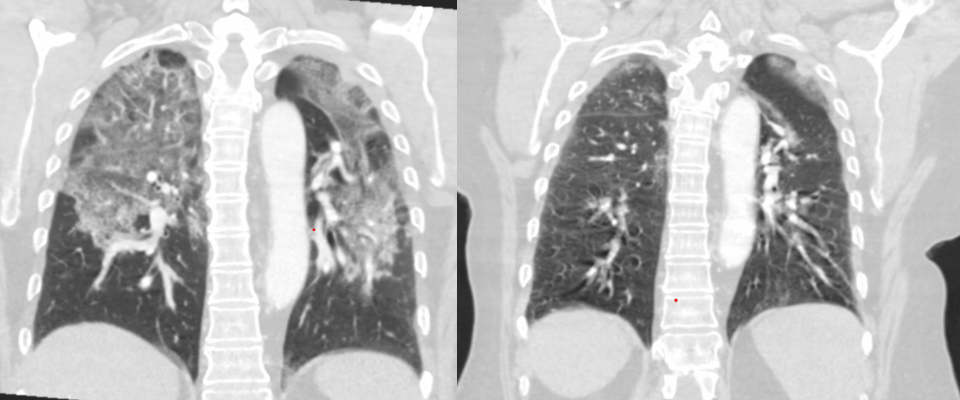
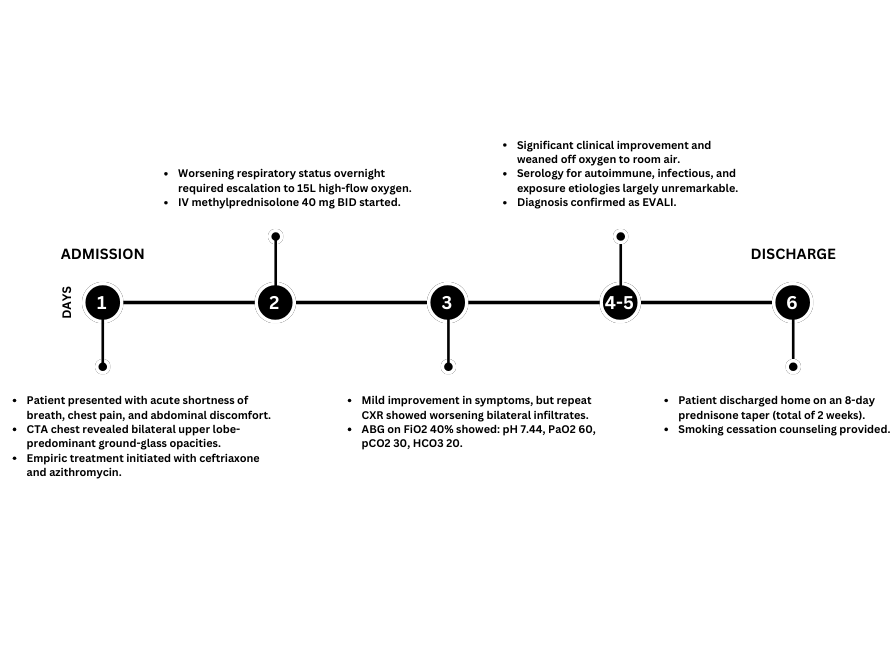
Case Presentation: E-cigarette or vaping product use-associated lung injury (EVALI) emerged as a significant public health concern during a 2019 CDC outbreak that affected 2,800 individuals and caused 68 deaths nationwide. While EVALI primarily affects young males, it manifests with respiratory, gastrointestinal, and systemic symptoms that can mimic conditions like pneumonia or COVID-19, creating diagnostic challenges. This report describes an atypical case of EVALI in a female patient who developed severe, rapid-onset hypoxia following first-time vaping.A 62-year-old female with a history of T2DM, HTN, HLD, MASH liver cirrhosis, CAD, and a 15 pack-year smoking history presented with acute shortness of breath, “twisting” chest pain, and abdominal discomfort. On admission, she was tachypneic and hypoxic, requiring 3L to maintain an oxygen saturation of 87%. Labs revealed neutrophilic leukocytosis (WBC 16.24 k/µL), mild anemia (Hgb 10.2 g/dL), hypokalemia (K 3.0 mmol/L), hyperglycemia (BG 168 mg/dL), procalcitonin elevation (0.10 ng/mL), elevated lactate dehydrogenase (LD 447 U/L), and inflammatory markers—C-reactive protein (CRP 22.3 mg/dL) and erythrocyte sedimentation rate (ESR 106 mm/h). Chest CTA revealed extensive bilateral ground-glass opacities, predominantly in the upper lobes.Within 24 hours, her condition deteriorated, with hypoxia worsening to require 15 liters of high-flow oxygen. She received empiric treatment with ceftriaxone and azithromycin for presumed community-acquired pneumonia. However, several factors suggested a non-infectious etiology: the absence of fever, persistently low procalcitonin (0.12 ng/mL), and negative blood and sputum cultures. Pulmonology consultation led to an extensive workup for autoimmune and exposure-related causes, which proved unremarkable. Further history revealed that the patient had switched from smoking to vaping one week before symptom onset. Treatment with corticosteroids (methylprednisolone 40 mg IV twice daily) produced dramatic improvement within 72 hours. Follow-up imaging showed significant reduction of inflammatory infiltrates. After six days of steady improvement, she was discharged on an oral prednisone taper and received smoking cessation counseling.
Discussion: EVALI remains a diagnosis of exclusion, requiring both a history of vaping and high clinical suspicion—particularly after ruling out infectious and autoimmune causes. This case presents several distinctive features: the patient was an older female without prior lung disease who experienced rapid hypoxic progression within one week after first-time vaping. Bilateral ground-glass opacities on imaging provided a crucial diagnostic clue, while thorough history-taking revealed vaping as the probable trigger. The case posed unique management challenges, including balancing steroid-induced hyperglycemia with pre-existing uncontrolled diabetes. Follow-up imaging documented the patient’s recovery. Additionally, this case demonstrates EVALI’s broadening demographic reach beyond its typical presentation in younger males.
Conclusions: This case highlights the critical importance of considering EVALI in patients presenting with acute hypoxia and bilateral pulmonary infiltrates—especially those with recent vaping exposure. Early corticosteroid therapy leads to improvement. With the rising prevalence of vaping, heightened provider awareness and robust public health initiatives are essential.