Background: Inpatient subspecialty consultation is one of the most common physician practices in the care of hospitalized patients. As per a CMS report, approximately 33,000 inpatient consultation occurred per day in 2008 costing Medicare approximately $1.9 billion. Common reasons for requesting a consultation include assistance with treatment, diagnosis, and request for a procedure. Consult quality affects the timeliness of treatment, tests performed, appropriateness of diagnosis and discharge. Majority of consultation request in the US is done via telephone (~76%) which makes it difficult to track quality and characteristics.
Purpose: Electronic consultation (e-Consults) are asynchronous, consultative, provider-to-provider communications within a shared electronic health record (EHR). In this abstract, we report utilization and outcome of an inpatient e-Consult implementation.
Description: Before implementation of the e-Consult process in 2017, consulting subspecialty services was a manual process external to the EMR. The process was very susceptible to misses, errors and resulted in frequent complaints of consult delays. To improve consult trackability, workflow, timeliness, and quality we developed the e-Consult tool into the EMR. Requesting provider were required to input their name, callback number, priority level (routine, urgent or life threating), and a brief reason for the consult. Option to page consult service automatically in addition to routing consult request to specialist team message box was also available. Provider consultation policy was created to clarify response expectation based on consult priority level.
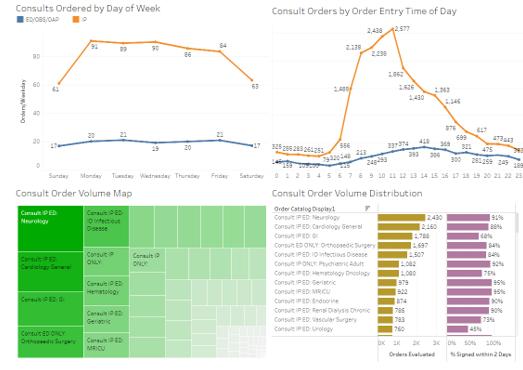
A total of 81 inpatients and emergency department (ED) subspecialty e-Consult orders were created and implemented. During the ten month study period (1/1/2018 to 10/31/2018) a total of 30,407 e-Consults were ordered on an average 100 e-Consults a day. Seventy-five percent of consults were ordered between 7 AM and 4 PM. Inpatient e-Consults rate dropped by 29%-30% over the weekend whereas ED e-Consult rate did not show significant variability. Nineteen percentage of e-Consults were ordered from the ED. Top three consulted services were Cardiology (2,919 e-Consults) and Gastroenterology (2,440 e-Consults) followed by adult Neurology (2,430 e-Consults). Internal Medicine specialties were responsible for 55% of e-Consults. Psychiatry accounted for 5% of e-Consults, whereas surgical specialties accounted for 20% of e-Consults. Two percent (755) e-Consults were ordered as life threating, majority 66% (19,989 e-Consults) were ordered as an urgent e-Consults and rest requested as routine. Quality of consult service was evaluated based on the percentage of signed notes within 48 hours of e-Consult order placement. Overall 82% of e-Consult notes were timely. For Internal Medicine 86% percent notes were in compliance whereas Surgery Department (excluding Orthopedic and ENT surgery) compliance with e-Consult timeliness was noted to be around 62 %.
Conclusions: e-Consults in the outpatient setting is relatively common but not well studied in the inpatient setting. In this abstract, we describe the utilization, pattern, priority, quality, and timeliness of consults utilizing the e-Consult process. Our implementation of e-Consult is not only novel but also demonstrates excellent and universal acceptance and usage.