Background: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are commonly-used antihypertensives which, despite renoprotective properties, can contribute to acute kidney injury (AKI)(1). Iodinated contrast media may also precipitate AKI, namely contrast-induced nephropathy (CIN), which has been associated with adverse patient outcomes(1–3). ACE inhibitors and ARBs are often held in the setting of iodinated contrast administration. While many studies(4–12) have addressed the impact of ACE inhibitors and ARBs on CIN following coronary angiography, fewer studies have addressed this question with contrast-enhanced CT scans(13,14), with conflicting results in both cases. We designed a retrospective study to determine the contribution of ACE inhibitors and ARBs to CIN following routine CT imaging studies.
Methods: We extracted our institutional data from adult inpatients with an eGFR between 15-60 ml/min/m2 and who received standard CT or CT angiography (CTA) studies of the chest, abdomen, and/or pelvis, or CTA studies of the cerebral vasculature over 2013-2018. We defined AKI as an increase in serum creatinine (sCr) of at least 0.3 mg/dL, or 25%, within 2-4 days after the CT scan. Patients were excluded if (1) sCr was unavailable prior to or at admission, on the day of CT scan, or on days 2-4 following the CT scan, (2) sCr was at least 0.5 mg/dL or 50% higher than the baseline or admission value on the day of CT scan, (3) the patient received contrast other than oral or chest tube administration within 4 days of the CT scan, or (4) there was a history of end-stage renal disease or renal transplant. Patients were included in the exposure group if they received an ACE inhibitor or ARB on the day of the CT scan or within the four subsequent days.
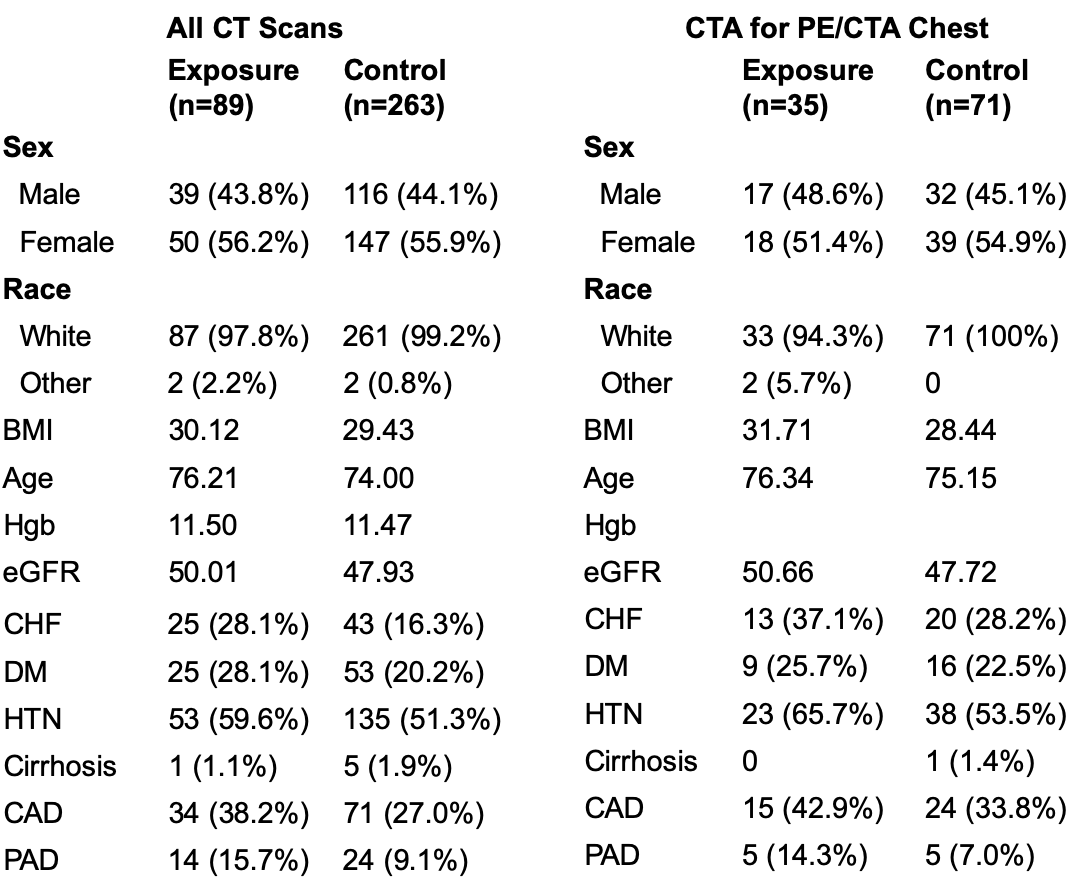
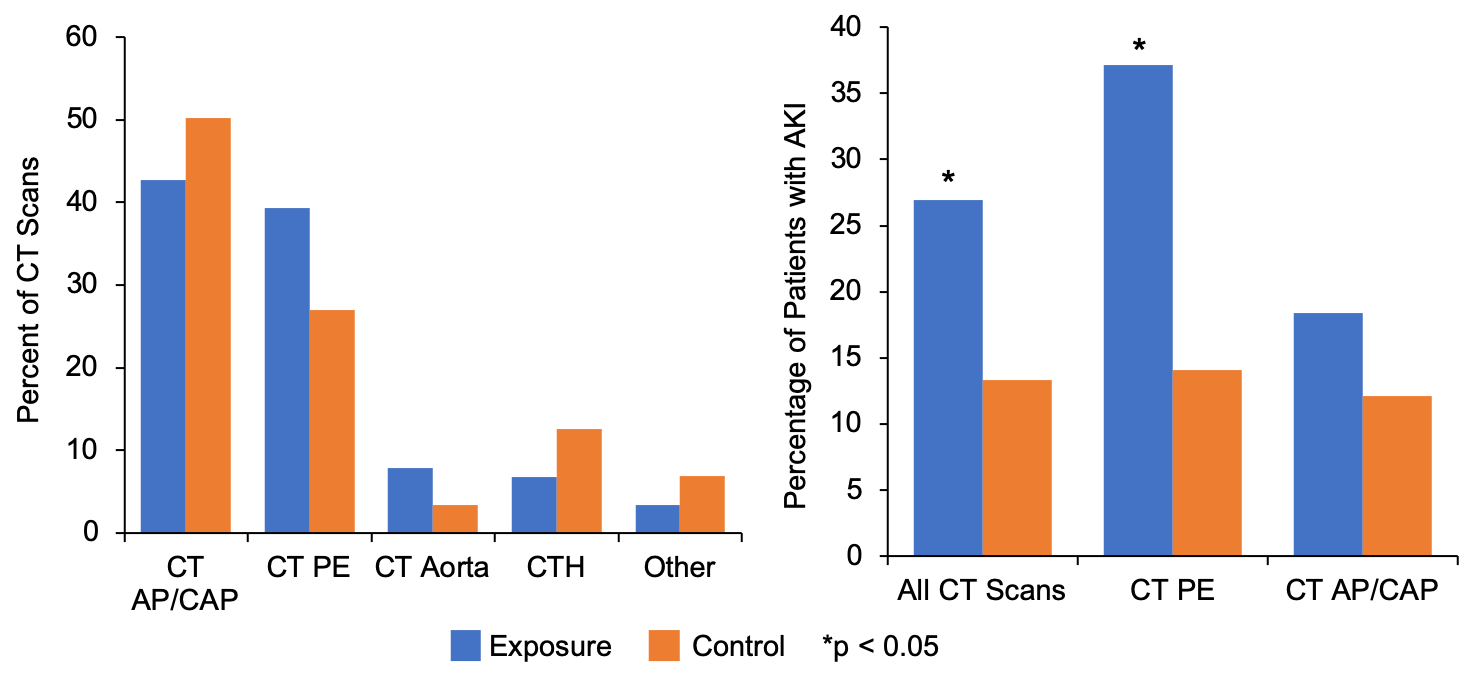
Results: Baseline characteristics are outlined in the attached figures. The study groups were well-matched for demographic characteristics. Mean eGFR was slightly higher in the exposure group, though with a larger proportion of relevant medical co-morbidities. AKI was observed in 24/89 (27%) patients in the exposure group and 37/263 (14.1%) patients in the control group (p = 0.002, Chi-squared test). Statistical significance was observed after correction for eGFR and the selected medical co-morbidities using a multivariable logistic regression model (OR 2.67, p = 0.003, Wald test). Since the types of CT scans also differed, we stratified the results by scan type. A significantly higher incidence of AKI in the exposure group was only observed for patients who received CTA of the chest (13/35 versus 10/71, p = 0.007 by Chi-squared test).
Conclusions: Our study suggests that administration of ACE inhibitors or ARBs following CT scans increases the risk of CIN. A statistically significant increase in AKI remained after adjusting for between-group differences in eGFR and selected medical co-morbidities that had been associated with CIN in prior studies(1,4,15,16), strengthening our confidence in this conclusion. Interestingly, this observation held only for CTA of the chest, which may be explained by the dose of contrast administered, or differences in medical indications for different studies. This study was limited by the retrospective and observational design, which poses a risk for selection bias. These groups were very different in size, presumably because ACE inhibitors or ARBs were held in the setting of contrast administration. Generalizability is limited based on the single-center design and predominantly Caucasian patient population.