Background:
Emergency department (ED) crowding has been shown to contribute to increased medical errors and poor patient outcomes. Efforts to reduce ED crowding often involve decreasing time between patient arrival and transfer to the hospital floor. However, efforts to improve ED throughput may have the unintended consequence of rushing triage decisions, leading to inappropriate triage of critically ill patients to the floor and unanticipated transfers to the intensive care unit (ICU).
Methods:
Since January 2010, the Division of Hospital Medicine at a 600‐bed academic medical center has made efforts to improve ED throughput for admitted patients. Specifically, strategies have focused on decreasing the time between the ED's decision to admit the patient and when admission orders are written. As admitting physicians use this time to assess the patient in the ED and determine admit location to the floor, step‐down, or ICU, decreasing this assessment time could affect patient outcomes. Utilizing a retrospective cohort design, we evaluated all patients admitted through the ED to a medicine floor from January 2010 to May 2012. Our predictor variable was time from decision to admit to admission orders, and our outcome variable was unanticipated transfer to the ICU in the first 24 hours of arrival to the floor. We considered the effects of ICU census and month of study period as covariates in our analysis.
Results:
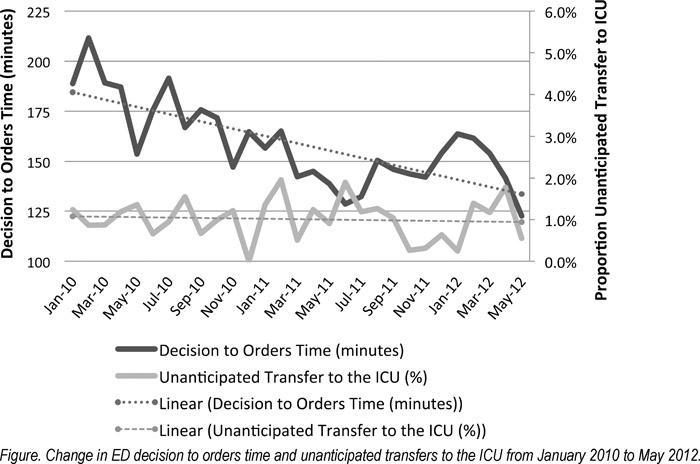
Over the 29‐month study period, 10,042 patients were admitted through the ED to a medicine floor, and mean time from decision to admit to admission orders decreased by 52 minutes (95% CI, 44–59 minutes; P < 0.001). We identified a total of 100 patients (1%) with an unanticipated transfer to the ICU within 24 hours of admission to the floor, and the monthly rate of unanticipated transfers to the ICU did not change significantly over time (P = 0.93; Figure). The overall mean decision to orders time did not differ significantly between those who had an unanticipated transfer and those who remained on the floor (175 minutes [95% CI, 149–202 minutes] vs. 159 minutes [95% CI, 157–161 minutes], P = 0.14). After accounting for study month and daily ICU census, the odds of an unanticipated transfer to the ICU decreased by 1.3% for each 10‐minute decrease in time from decision to admit to orders. Although this trend was not statistically significant (OR, 0.987; 95% CI, 0.972–1.002; P = 0.12), the upper end of the 95% CI excludes any significant increase in unanticipated transfers as a result of improved throughput.
Conclusions:
Efforts to reduce ED throughput must be balanced by the unintended consequences of rushed triage decisions. In our population of patients admitted through the ED to the medicine service, efforts to increase ED throughput have not resulted in increased unanticipated transfers to the ICU.