Background: Poor coordination between hospital and outpatient care worsens health outcomes, and increases preventable hospitalization and health care expenditures, especially for socioeconomically disadvantaged populations. Evidence of the effects of current programs to improve care coordination is mixed, and there is little data on how their impact may differ for hospitalizations for ambulatory care-sensitive conditions (ACSCs) compared to other conditions (non-ACSCs), and across populations. The Comprehensive Care Program (CCP) at the University of Chicago utilizes a novel approach to care coordination in which physicians provide both ambulatory and hospital care to Medicare beneficiaries at increased risk of hospitalization. The CCP has been found to reduce hospitalizations overall and among traditional Medicare patients, but not in patients with both Medicare and Medicaid (dual-eligibles). This paper examines whether the effect of the CCP varies for ACSCs and non-ACSCs, with stratification across dual-eligible insurance status.
Methods: In this secondary analysis of a randomized trial of the CCP, we examined Medicare claims data for hospitalizations during the year after randomization; enrollment took place between 2012 – 2016. ACSCs were classified using the Agency for Healthcare and Research Quality guidelines. We used a negative binomial regression to compare the adjusted incidence rate ratio (IRR) of hospitalizations for ACSCs and non-ACSCs among duals and non-duals, controlling for patient characteristics at baseline; age, sex, health status, ESRD, functional limitations, and pre-existing primary care doctor.
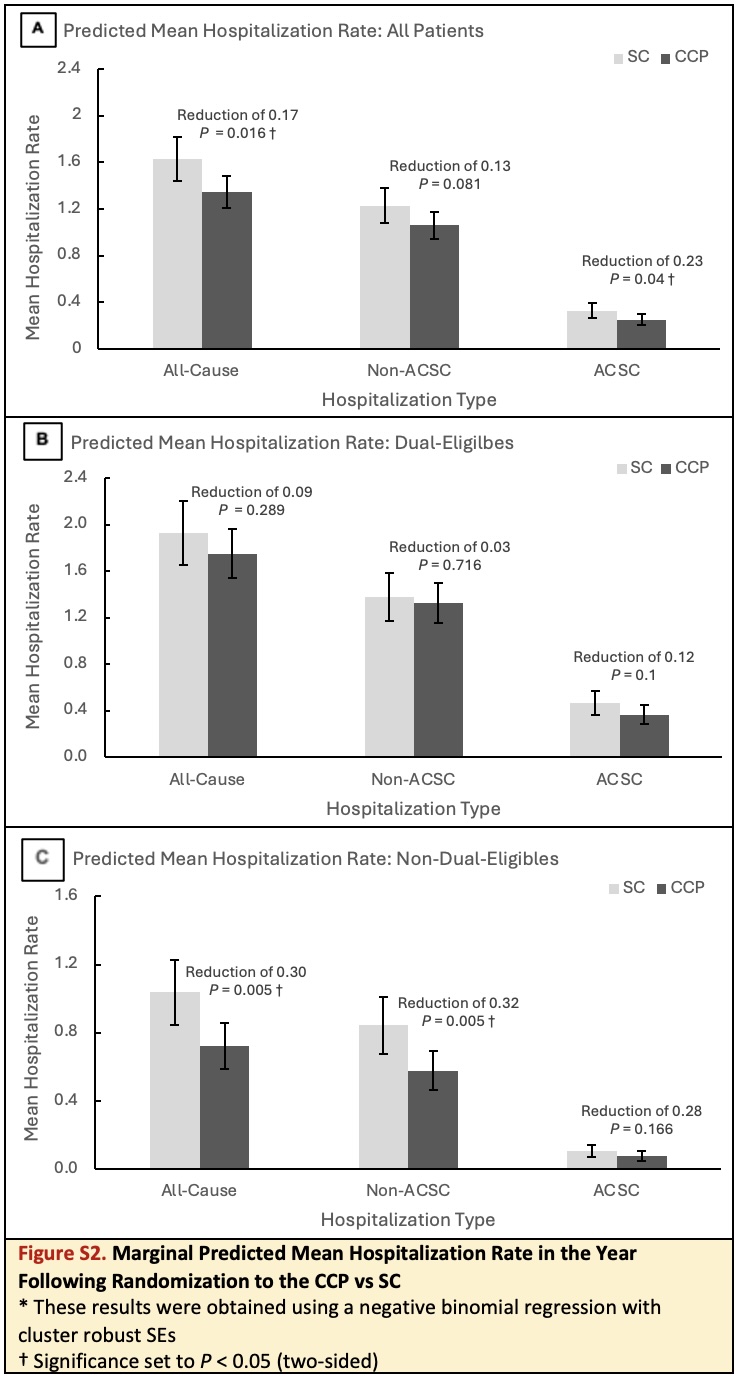
Results: The cohort included 1,916 patients: 957 in standard care (SC) and 959 in the CCP. Of the 3969 total hospitalizations, ACSCs accounted for a small proportion overall (22.7%), but represented a larger share of hospitalizations among duals compared to non-duals (24.5% vs. 16.4%; p < 0.01). The overall reduction of hospitalizations in the CCP was a combination of a significant reduction in ACSC hospitalizations (0.77; 95% CI, 0.59 - 0.99; p = 0.04) and a non-significant trend towards lower non-ACSC hospitalization (0.87; 95% CI, 0.74 – 1.02; p = 0.08). When exploring these effects across populations, the CCP showed a similar trend towards a reduction in ACSCs among both duals and non-duals, though neither was statistically significant. For non-ACSCs, however, the CCP led to a large and significant reduction among non-duals (0.68; 95% CI, 0.52 – 0.89; p < 0.01), with no effect among duals.
Conclusions: The provision of hospital and ambulatory care by the same physician in the CCP reduced hospitalizations for ACSCs among high-risk Medicare beneficiaries. Large and statistically significant reductions in non-ACSCs among non-duals suggest that many hospitalizations classified as non-ACSCs may be preventable and raises questions as to how the CCP prevents them. It remains unclear why no significant effect was seen among duals.