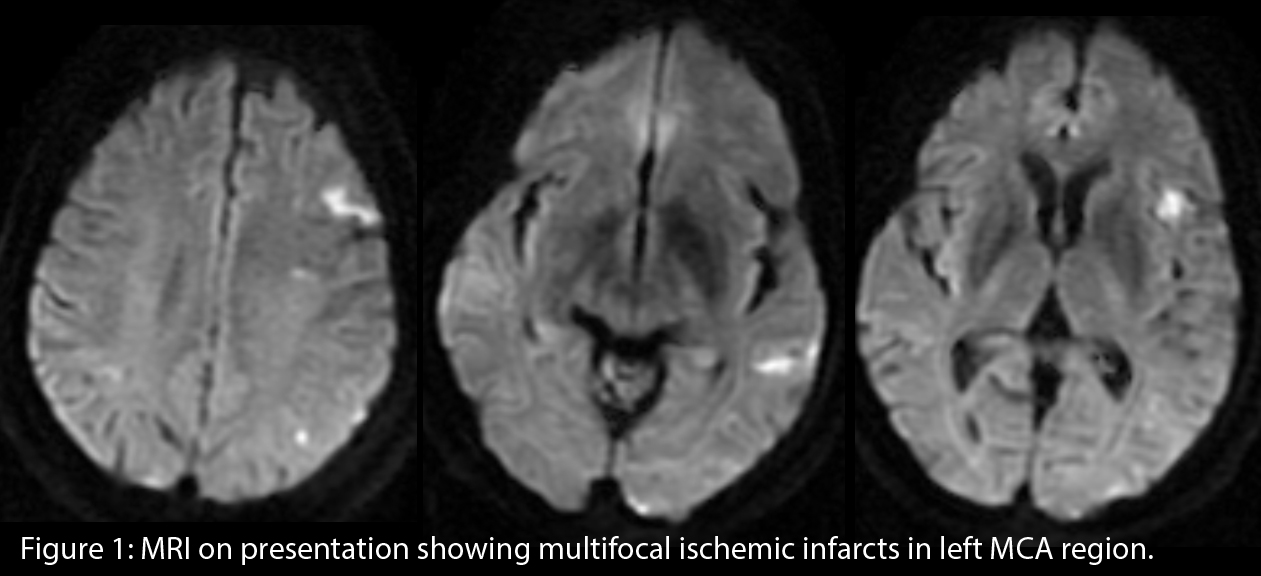
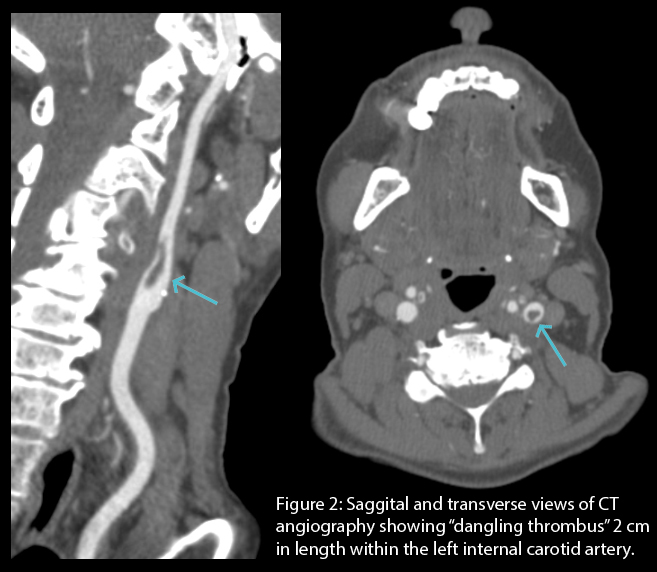
Case Presentation: A sixty two year old woman with good baseline functional status, with medical history of: asthma, active tobacco smoking, and estrogen replacement therapy for menopausal symptoms. She presented with acute onset difficulty speaking starting one day prior. On examination she exhibited obvious expressive aphasia with severe word finding difficulties. The ability to understand speech and follow command was fully intact. No extremity weakness noted. She was admitted for acute cerebrovascular accident. No chemical thrombolysis was administered due to presentation being outside time window. Magnetic resonance imaging (figure 1) confirms multi-focal ischemic infarcts in the left middle cerebral artery distribution. The distribution was suspicious for an embolic etiology. Computed tomography angiography of the brain and neck (figure 2) revealed a “dangling thrombus” two centimeters in length within the left internal carotid artery with a peculiar, hanging appearance. This was likely the embolic origin. The thrombus itself was not causing flow limitations. Decision was made to manage the carotid thrombus with anticoagulation and medical therapy instead of endarterectomy, as surgical manipulation is associated with high risk of embolization with this type of thrombus. She was started on aspirin, statin, and rivaroxaban. Transthoracic echocardiography did not show any intra-cardiac thrombus. Over the course of the next few days her symptoms dramatically improved; on day of discharge she was able to verbally communicate effectively, albeit still with some minimal residual expressive aphasia. Long term plan is to continue medical therapy for at least three month at which time surveillance angiographic imaging will be performed to evaluate for thrombus resolution.
Discussion: This patient suffered an embolic stroke with the source being an internal carotid thrombus of peculiar morphology. Interestingly, there is minimal to no background atherosclerotic disease. Systemic estrogen therapy was suspected to be causing hyper-coagulability. Although the data on this subject is not conclusive, it does overall support a positive correlation. After risk versus benefit discussion, the patient elected to cease hormone replacement therapy. Tobacco cessation was also advised. Carotid endarterectomy was considered, however the risk of intra-operative embolization was considered too great, as the thrombus appeared to be only weakly adherent to the vessel wall. Fortunately the patient did quite well clinically with aspirin and anticoagulation. P2Y-inhibitor was deferred in order to avoid excessive bleeding risk. If follow up imaging shows complete resolution of the thrombus then anticoagulation and/or antiplatelet will likely be discontinued.
Conclusions: Suspicion for occult arterial thrombosis should be low for patients with stroke and hyper-coagulable risk factors. Endarterectomy is the standard of care for carotid disease. However, in the case of this loosely adherent clot with high surgical embolic risk, medical therapy alone is a reasonable approach.