Background: Endoscopies are commonly performed in the inpatient setting, and successful completion frequently requires close coordination among nurses, hospitalists, gastroenterologists, and anesthesiologists. Given the complexity of this multidisciplinary involvement, as well as variability in patient factors like clinical stability and presentation, endoscopies are prone to delays. These delays may cause frustration amongst care providers and patients, patient discomfort from prolonged nil per os time, and excess costs from lengthened hospitalizations.
Purpose: We sought to reduce avoidable inpatient endoscopy delays by optimizing workflow, scheduling, and staffing in our large, urban university medical center.
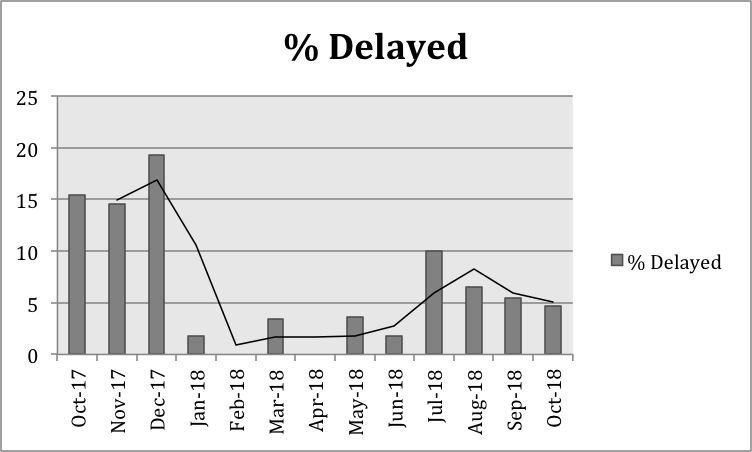
Description: A survey of hospitalists at our institution identified endoscopy as a common contributor to delayed patient discharge. Representatives from gastroenterology, anesthesiology, hospital medicine, inpatient nursing, and endoscopy nursing were engaged to create a multidisciplinary team to evaluate and intervene upon these delays. Root-cause analysis demonstrated multifactorial causes of endoscopy delays, and baseline data showed that 16.4% of inpatient endoscopies were delayed due to reasons characterized as avoidable, with an average length of delay of 1.22 days. The identified highest impact contributors to avoidable reasons for delay were endoscopy nursing availability, anesthesia provider availability, and volume of competing scheduled outpatient procedures. Three interventions to address these common causes of delay were implemented. First, dedicated anesthesiologist availability for inpatient endoscopy cases was provided on prespecified weekdays. Second, the endoscopy nursing staff instituted later and extended shifts to accommodate more procedures. Third, the on-call gastroenterologist reduced the number of daily scheduled outpatient endoscopic procedures, allowing for increased endoscopy suite allocation to inpatient procedures. The proposed interventions underwent several plan-do-study-act cycles to identify optimal implementation, with a target goal of 5% delay rate. Following implementation of these interventions, the average rate of avoidable endoscopy delays fell to 3.5% while average total endoscopies per month remained constant.
Conclusions: A novel inter- and multidisciplinary collaboration to optimize staffing and scheduling resulted in significant and sustainable reductions in avoidable inpatient endoscopy delays at our large, urban university hospital. Improvement required a multi-pronged approach to address key root causes and engender culture change. Continued efforts to quantify outcomes measures such as length of stay reduction, nil per os time, and cost evaluation are planned.