Background: Cost associated with diagnostic testing contributes greatly to the rising cost of health care in the United States (Bindraban et al, 2018). There is evidence to suggest that up to 20% of lab testing is unnecessary (Bindraban et al, 2018).Main Line Health (MLH) is a health system in suburban Philadelphia made up of four acute care hospitals, including Lankenau Medical Center (LMC), is a community academic center. At LMC, internal medicine residents are involved in the care of approximately half of the patients on the hospitalist services. In recent years, MLH has used an audit and feedback approach to educate hospitalists on their individual practice metrics including lab utilization with success in reducing daily lab ordering. Trends across all acute care sites have shown less impact on rates of daily common lab ordering at LMC when compared to the non-academic sites. Feedback revealed that academic hospitalists at LMC did not feel their practice-based data was actionable due to difficulty distinguishing hospitalist practice patterns versus resident actions and ordering behaviors.
Purpose: Improve engagement from academic hospitalists in review of practice-based metrics, as well as promote better awareness of individual practice habits and encourage behavior change.
Description: Audit and feedback data for LMC academic hospitalists was separated based on whether residents were involved in patient care or if the hospitalist was caring for the patient independently. Data on daily common lab ordering and complete metabolic panel (CMP) use was analyzed for academic hospitalists with resident-associated encounters removed.
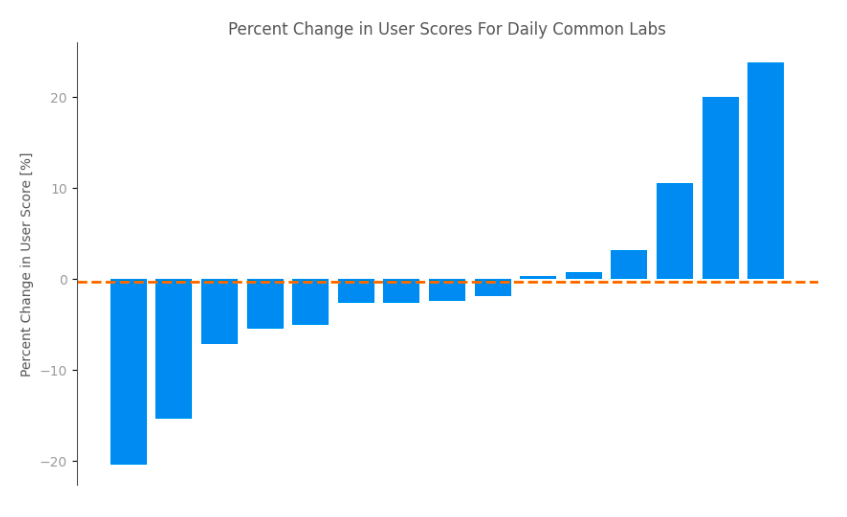
Conclusions: Across the group, the rate of ordering daily common labs for academic hospitalists was 1% lower with resident-associated encounters excluded and the rate of complete metabolic panel utilization was 20% lower with resident-associated encounters excluded. No academic hospitalist data remained the same after excluding resident-associated encounters. The maximum relative change for an individual was approximately 20% for daily common lab ordering (Figure 1) and approached 100% for CMP ordering (Figure 2). Given this wide range of individual practice variation, all future audit and feedback data for LMC academic hospitalists will be separated from resident-associated encounters. We anticipate that academic hospitalists will find the data more useful for personal improvement and will allow them to better role model cost conscious care for trainees.