Background: Pressure injuries are tissue damage caused by pressure and shear. Susceptible patients are the elderly, acute, critically ill and malnourished. Pressure injuries severely deplete hospital performance measures in the U.S. Currently, over 2.5 million patients develop pressure injuries at a national cost of about $25 billion each year and are implicated in 50,000 deaths. Medicare has instituted a series of payment reductions over the past decade to incentivize prevention, but systems are slow to respond. A recent data report by Medicare indicates that pressure injury rates have increased 58.4% since 2016. Existing best practice guidelines for pressure injury prevention may either lack efficacy, are not being implemented effectively because of their overall cost and labor intensity, or both.
Purpose: We aim to provide timely, relevant education centered on new, innovative evidence-based technologies and quality improvement interventions for pressure injury prevention in the hospitalized patient. We will illustrate the value of these interventions using data on the real-world efficacy and cost-effectiveness using studies run in parallel at hospitals in the U.S. and Australia known as the “BORDER” trials.
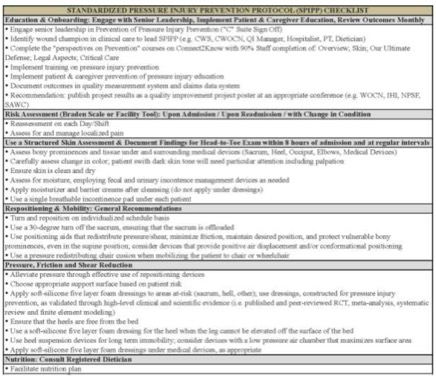
Description: The Standardized Pressure Injury Prevention Protocol (SPIPP) has been developed by members of the U.S. National, European and Pan-Pacific Pressure Ulcer Advisory Panels as a checklist to ensure that hospitals are adherent to best-practice guidelines and adopt best available technology. We will introduce SPIPP to hospitalists, along with quality improvement strategies to consider to increase the likelihood of adoption. Several key components of SPIPP will be reviewed with data of findings. First, we will introduce methods of standardized hospitalized patient risk-assessment using evidence-based instruments. Second, we will explore new evidence supporting the use of 5-layer prophylactic sacral dressings to reduce pressure injury rates by 30-80%. Third, we will explore how repositioning systems can systematically standardize positioning of an at-risk patient to reduce variability in exposure of soft tissue to pressure and shear. These components of SPIPP combined in a bundle with a patient-centered nutrition protocol can lead to overall reductions in pressure injuries, as witnessed through statistically significant, clinically meaningful, and cost-effective improvements from more than 1000-patient trials of hospitalized patients in the U.S. and Australia.
Conclusions: Hospital-acquired condition prevention programs centered on pressure injury care stand to address the prevention needs of one of the more costly and potentially fatal hospital-acquired conditions. Hospitalists should become familiar with the indications and use of new technologies for pressure injury prevention so that they can plan for integration and enhancement with existing quality improvement bundles. Thereby, hospitalists can effect positive change in patient outcomes that lead to fewer payment penalties, decreased patient length-of-stay and fewer readmissions caused by chronic wound care.