Background: The Cost Savings Reinvestment Program (CSRP) was created to benefit both the School of Medicine (SoM) and Stanford Health Care by incentivizing physicians to develop and assist with the implementation of initiatives that reduce hospital costs while maintaining or enhancing the quality of care provided to hospital patients. Cost savings realized from successful initiatives are shared with SoM Departments and may be used for purchase of equipment and supplies and/or to fund research projects or used for continuing education and other program development activities. The expectation is that the funds will benefit the front-line physician(s) that originated and implemented the successful initiative and cannot be used as direct or indirect salary or compensation support.
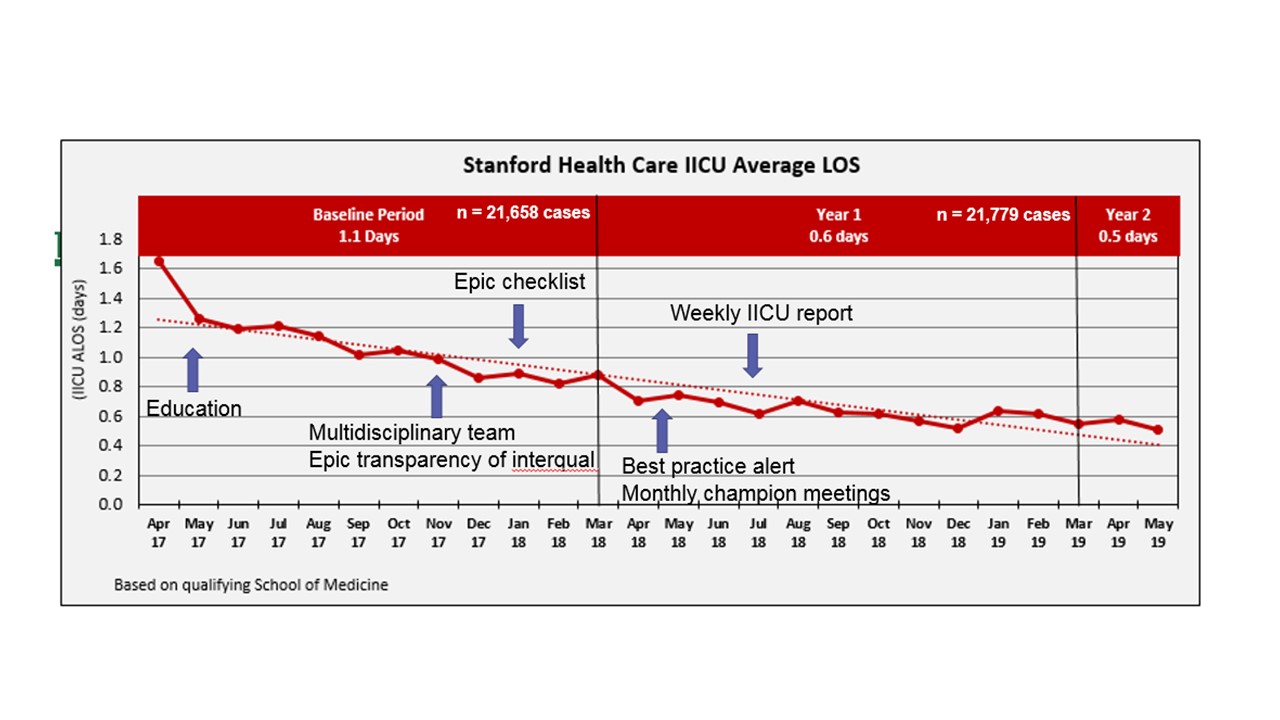
Purpose: Patients spend more time on intermediate ICU level (IICU) level of care than is medically necessary. IICU costs are significantly more per day than acute level of care. Audits in November 2017 using InterQual® – McKesson Level of Care Criteria showed 45% potential inappropriate IICU use. We describe a CSRP project identified and created by hospital medicine physicians that brings together nursing, case management, and physician champions while also utilizing clinical decision support to decrease inappropriate use of IICU in 15 divisions hospital wide.
Description: Problem analysis revealed top barriers to inappropriate IICU use were lack of transparency of current level of care and inconsistent discussion by providers regarding appropriate use of IICU. We engaged physician champions in participating divisions to promote appropriate IICU use with extensive multidisciplinary rollout hospital wide. We did weekly audits to measure inappropriate IICU use and sent these results to the physician champions. Weekly IICU use by service line was also sent to all participating service lines. To address lack of transparency of current level of care, we automated the current level of care designation into patient lists that were found in the EMR and rounding reports. We also made the InterQual® – McKesson Level of Care criteria visible to all in the EMR (whereas it used to be in a separate system only seen by case management). To address inconsistent discussion by providers regarding appropriate use of IICU, we partnered with case management and nursing to include discussion of appropriate IICU use as part of standard work. We created EMR best practice alerts to promote daily assessment of appropriate IICU use by providers. Balancing measures of rapid response teams, codes, and mortality were monitored during the project.
Conclusions: From April 2018-March 2019, IICU LOS decreased by 0.5 days overall in 15 divisions compared to the previous year. InterQual® – McKesson Level of Care Criteria showed significant improvement of appropriate IICU use from 50% to 80%. Cost savings estimates of accommodations were $5.7 million over one year. We believe initiatives like CSRP will play a key role to engage front line physicians to identify and design high value care programs. Front line physicians in collaboration with other disciplines that took this challenge head on, incentivized by potential cost savings reinvestment that can help drive physician education, quality improvement, or research programs.