Background: Identifying discharge barriers, reducing length of stay (LOS) and optimizing the observed over expected (O/E) ratio for LOS are crucial in healthcare management. Addressing obstacles—DME needs, medical issues, diagnostic/procedure delays, administrative hurdles—can streamline discharge, enhancing outcomes, optimizing resources, cutting costs, and improving hospital efficiency. Effective discharge planning, interdisciplinary collaboration, and patient education are vital for mitigating barriers and achieving shorter LOS.
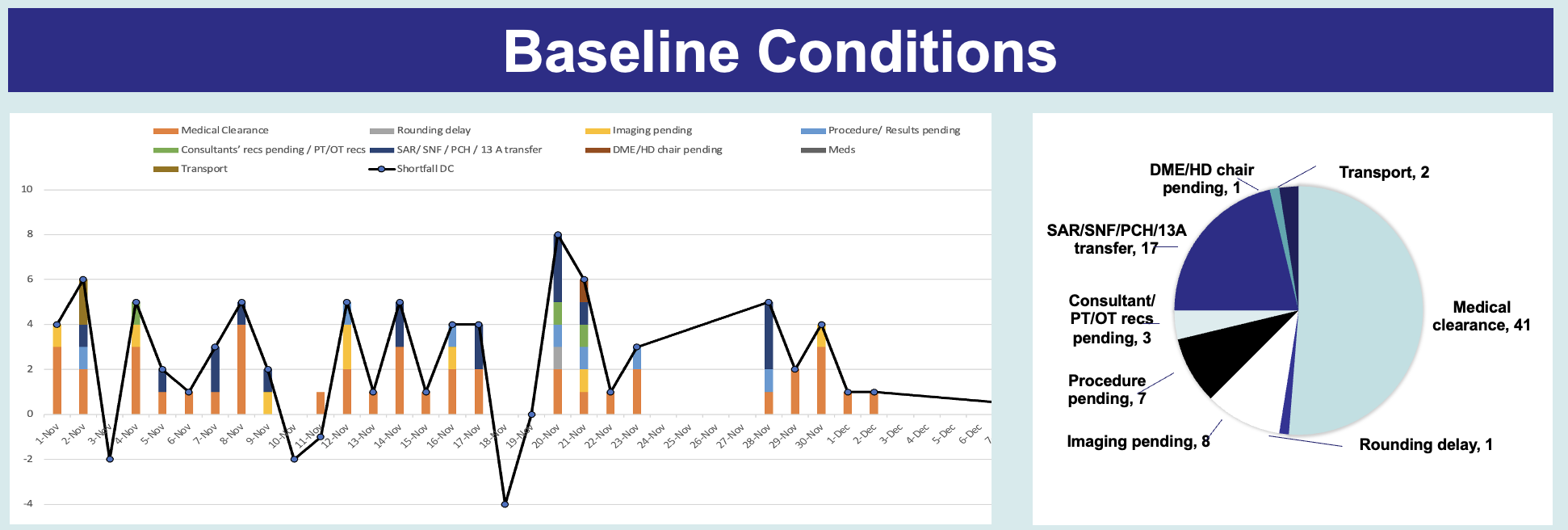
Methods: We retrospectively analyzed all expected discharges in November–December 2022 to discern patterns between patients who were or were not discharged. We examined charts of patients who remained hospitalized despite being on the list for discharge, to identify and understand any barriers. To mitigate discharge delays, we initiated a pilot program of 14:00 discharge rounds in July 2022 where provider teams review patient lists with care coordination to identify and address discharge barriers. To elucidate “medical clearance, we developed a “discharge planning” template, integrated as an EPIC smartphrase in progress and history and physical notes.Baseline Conditions: Among 218 anticipated discharges, 82 did not leave when expected. Fifty percent stayed due to medical clearance, and the reminder to delays in consultants’ recommendations (20.7%), imaging (9.7%), procedures (8.5%), transportation (2.4%), rounding (1.2%) and DME (1.2%).Test of Change: We assessed discharge rates before and after implementing discharge rounds and the discharge planning template.
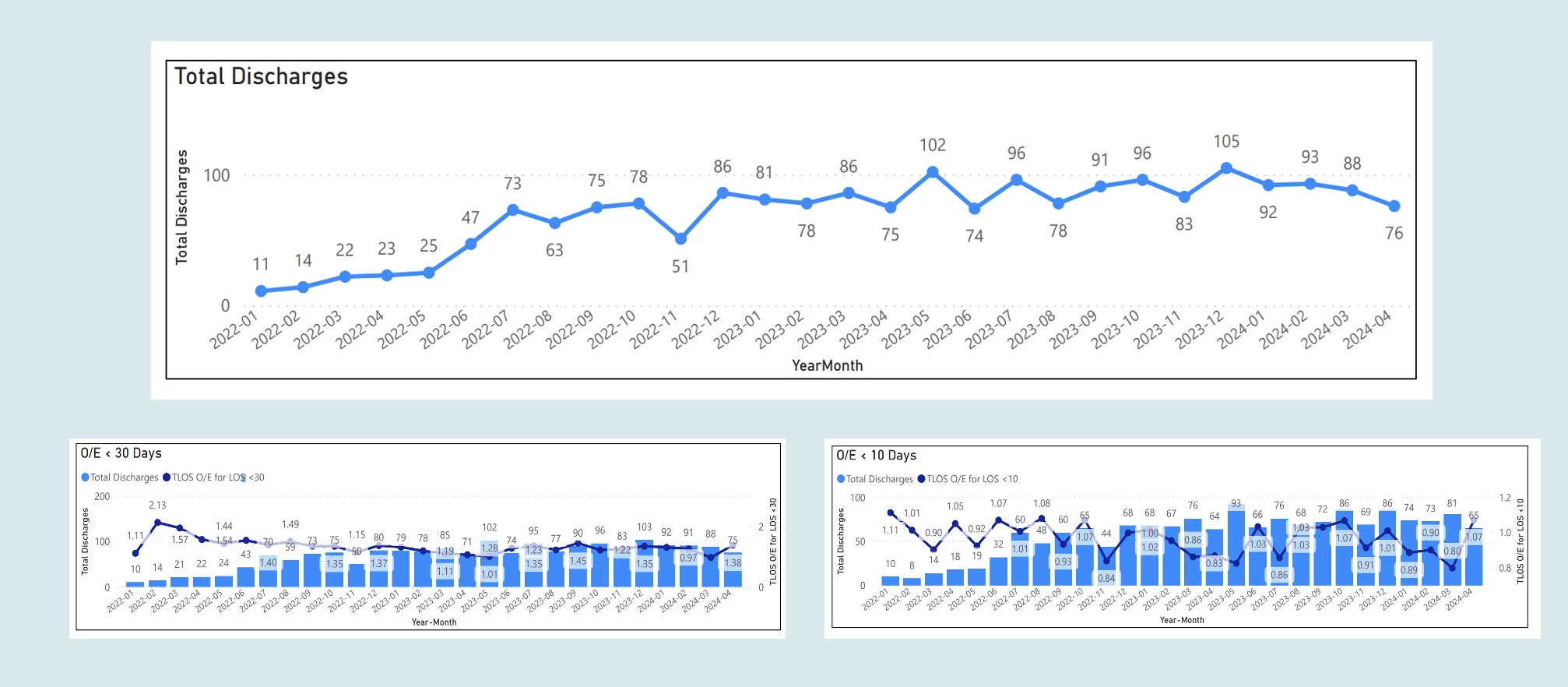
Results: Mean discharges per month increased from 24 (January–June 2022) to 92 (January–June 2023), a 3.5-fold increase. The observed-to-expected (O/E) LOS metric decreased: for stays < 10 days, the O/E ratio dropped from 1.01 (January–June 2022) to 0.90 (January–June 2023).
Conclusions: Efficient discharge planning allows for early determination of expected discharge dates, minimizing non-medical delays. Identifying discharge barriers via discharge rounds and a discharge planning template can optimize LOS O/E ratio by reducing patient LOS, leading to better health outcomes, cost savings, increased bed availability, enhanced service capacity, and reduced hospital workload.