Background: Unplanned readmissions in the U.S. healthcare system cost over $15 billion annually, a burden that increasingly impacts health systems as more patients transition to fully capitated models [1-2]. Despite evidence supporting the protective effect of post-hospitalization visits with primary care providers (PCPs), patient completion rates of these visits remain low [3-5]. Barriers include provider availability and perceived lack of necessity, with many patients opting to forego PCP visits in favor of specialists or missing appointments altogether [6-8]. To address these challenges, the UCLA Nudge Unit, in collaboration with Department of Medicine (DOM) Quality, implemented a novel intervention where post-discharge follow-up appointments were scheduled via video visits with the DOM scheduling team. These video visits were designed to engender social accountability to attend the appointment through a personal connection with the scheduler, and utilized a face-to-face commitment to improve appointment attendance rates.
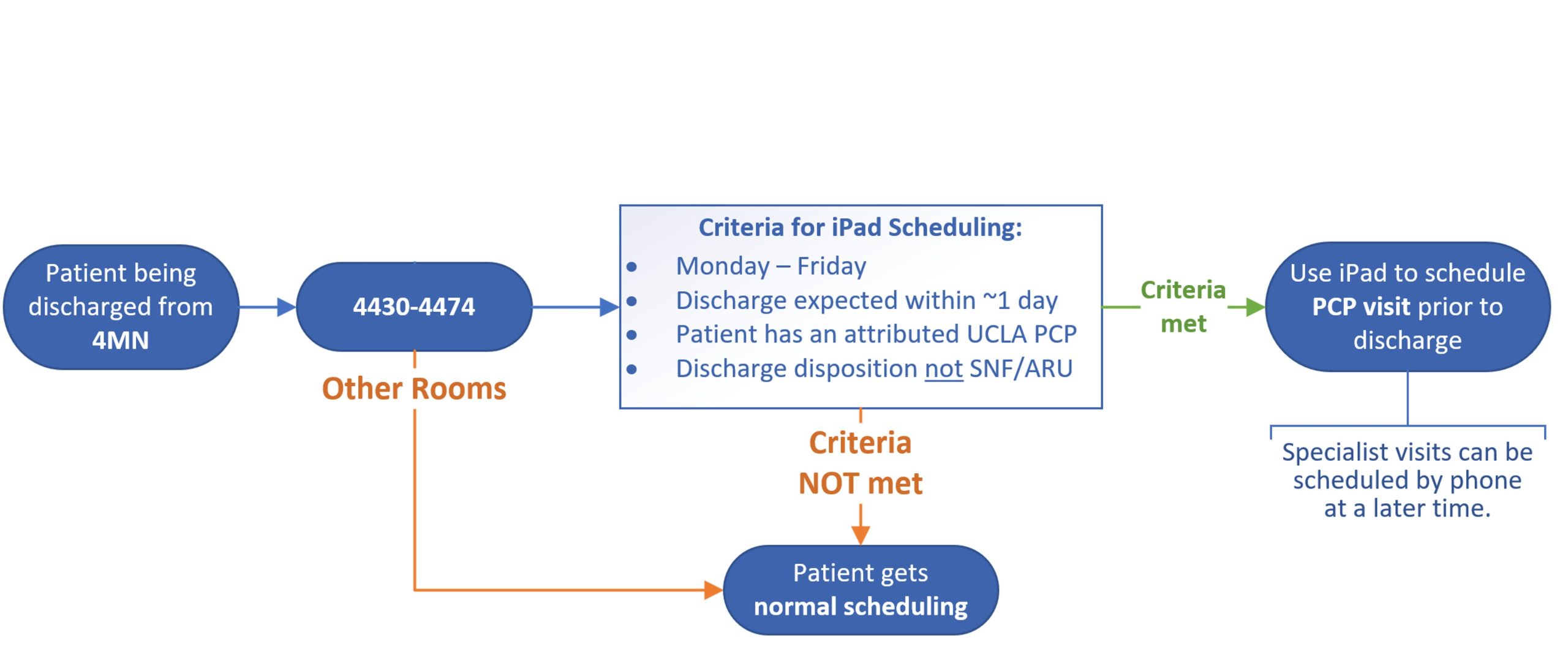
Methods: We implemented a room-based randomization scheme to evaluate this intervention: half of the rooms in one unit at the UCLA Santa Monica Medical Center were designated as ‘treatment’ rooms, with the remaining rooms in the unit serving as controls (Figure 1). Eligible patients included those discharged from treatment rooms, empaneled to a UCLA PCP or willing to empanel to one, not enrolled in hospice, and discharging home. Treatment group patients were identified by discharge nurses the day before their expected discharge, enabling the scheduling team to arrange appointments. On discharge day, floor nurses and care partners facilitated a Zoom video call between the patient and a scheduling team member using an iPad, allowing the patient to schedule their follow-up appointment synchronously. This is in comparison to the standard scheduling process whereby DOM schedulers call patients in the days following their discharge with pre-set appointments. The outcomes were having a post-discharge follow-up appointment scheduled and completed within seven days of discharge.
Results: A total of 41 patients were enrolled in this pilot RCT (14 in treatment group, 27 in control group; Figure 2). 86% (n=12/14) of patients in the treatment group had post-discharge follow-up scheduled within 7 days, compared to only 52% (n=14/27) of patients in the control group (p=0.02). 64% of eligible patients in the treatment group completed their 7-day post-discharge follow-up, compared to only 37% in the control group (p=0.11). The treatment group also experienced a lower no-show rate (7.14%) compared to the control group (11.11%), with most control no-shows being rescheduled within the 7-day window.
Conclusions: Compared to the standard post-hospitalization appointment scheduling method, this randomized pilot study of video-assisted appointment scheduling demonstrated a statistically significant increase in post-discharge scheduling rates (86% v. 52%) and a non-statistically significant increase in post-discharge appointment completion rates (64% v. 37%). Larger studies are needed to confirm these findings and support broader implementation.