Background: Background: Rapid response (RR) is a system in place to intervene when hospitalized patients experience acute deterioration in medical conditions.Problem Definition: Residents at LSU Shreveport/Monroe Family Medicine program have reported facing decision-making challenges and increased stress when called to manage rapid responses.Aim Statement: Enhance the rapid response management skills and confidence among the residents by at least 30% through a structured series of educational classroom-based and simulation sessions over a 3-month periodProblem Characterization:Lack of structured educationLack of frequent exposure to RRs due to an overlap of teams in managing RRs (including ED providers and other medical teams)
Methods: Methods: A Quasi-experimental study aimed to measure the residents’ perceived confidence and assess their knowledge and skills in managing rapid responses pre- and post-interventionIntervention: A structured series of educational classroom-based and simulation sessions based on the current guidelines and standard of care including the following topics:Altered mental statusSeizuresAcute neurologic deficitOpioid overdoseNon-redirectable agitation/combative behaviorChest pain (ACS/PE/Pericarditis/Aortic dissection)Dyspnea/HypoxiaArrhythmias (AFlutter/AFib w/ RVR, other tachyarrhythmias, bradyarrhythmias)GI bleedingAbdominal painDKA/HHS/hypoglycemiaAnaphylaxisHypertensive emergencyHypotension/ShockOutcome Metrics:Pre-intervention, a survey was used to measure the residents’ confidence and perceived self-level of knowledge and skills in managing RRs using a 5-point Likert scale. Also, quizzes with vignette-based multiple-choice and open-ended questions were administered to assess the residents’ knowledge of managing RRs at the beginning of each educational session.Post-intervention, in a similar fashion, a survey and quiz with vignette-based questions were used to measure confidence and assess the knowledge retained after completing the sessions.
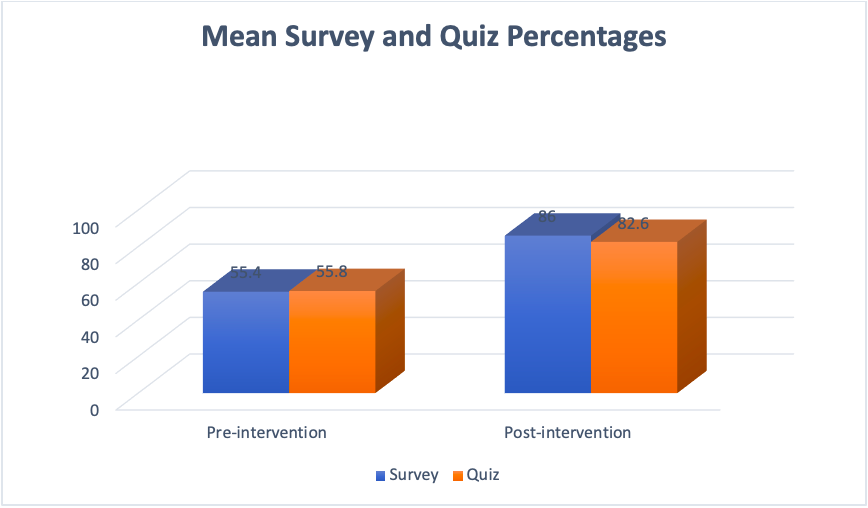
Results: Pre-intervention:18 residents completed the pre-intervention survey. The average confidence score on RR material was 2.77 out of 5 (55.4%). It is worth noting that mean scores varied based on resident year, with average scores of 2, 3.2, and 3.5 out of 5 for PGY-1, 2, and 3, respectively. All residents chose a 5/5 (extremely useful) when asked if they felt that the educational sessions would be useful to enhance their knowledge. The pre-intervention quizzes were administered immediately before each of the 4 educational sessions, and completion rates varied based on the availability of the residents during the sessions. The mean scores were 56%, 50%, 75%, and 42.2% for the 1st, 2nd, 3rd, and 4th sessions, respectively.Post-intervention:14 residents completed the post-intervention survey and quiz. The mean self-confidence was 4.3 out of 5 (86%), indicating a 55% increase in the perceived confidence among the residents. The average quiz score was 82.6%, indicating a 48% improvement in knowledge in managing RRs.
Conclusions: Structured education on RR management in our residency program was a recognized gap. The intervention helped to enhance the residents’ self-confidence and competence in responding to RRs and created a foundation for structured RR education, preparing the residents to practice Hospital Medicine confidently.We plan to develop strategies for sustaining the change by incorporating scheduled training sessions throughout the academic year.