Background: Nearly one-third of laboratory tests in hospitalized patients and up to 60% of routine, repeat lab tests are unnecessary. Unnecessary testing results in excess venipuncture, iatrogenic anemia, patient discomfort, excess costs, wasted lab resources, and a potential cascade of additional tests and interventions. Few academic medical centers, including our institution, have systematic lab stewardship programs, and the impact of one-off quality improvement initiatives are short-lived. When compared to peer academic medical centers, our institution orders significantly more lab tests per inpatient hospitalization.
Purpose: We created a comprehensive lab stewardship program to monitor lab utilization, safely and sustainably reduce unnecessary lab testing and costs, and improve the quality of care for patients. We describe our framework for developing this program here.
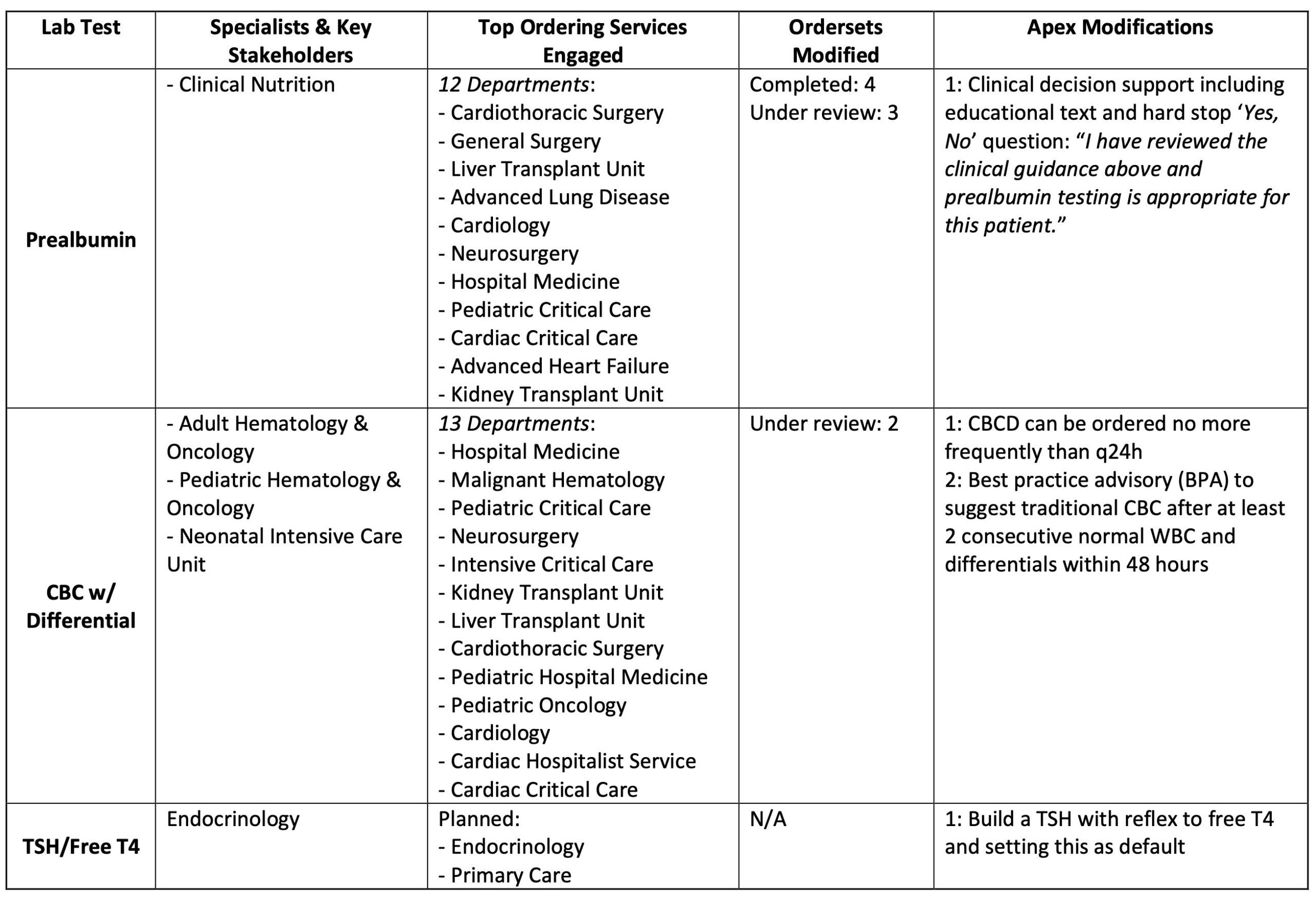
Description: We analyzed our institution’s lab tests by volume and cost, value-based care guidelines, evidence-based medicine guidelines, and potential for successful clinical decision support (CDS)-based interventions, and selected three pilot lab tests for year one: CBC with differential (CBCD), prealbumin, and free T4. To oversee our program, we established a lab stewardship governance committee with expertise in laboratory medicine, hospital medicine, informatics, quality improvement, and change management. For each pilot test, we met with content experts, created multimodal educational materials, designed electronic health record (EHR) modifications and CDS to reduce unnecessary lab testing, and identified top-ordering services. We then met with key stakeholders, including leadership from top-ordering services, quality and value, and clinical training programs, to review our recommendations, gather feedback, and ensure our educational materials and EHR modifications were clinically appropriate, minimally disruptive, and accounted for service-specific needs. Our educational campaign included presentations in a variety of venues to ordering clinicians. We also created high-yield summaries that were distributed electronically, displayed on computer screensavers, and posted throughout the hospital. EHR modifications included CDS within lab test orders, best practice advisories (BPAs) to reduce unnecessary repeat labs, and removal of pre-checked labs from ordersets where appropriate. To track our performance, we developed a dashboard with key metrics including total lab volumes, lab tests per admission and per admission-day, cost-savings, and balancing measures for each of the three lab tests. We designed the dashboard with filters to provide feedback on service- and department-specific performance, enable stakeholders to narrow in on their population of interest, and allow adding additional lab tests in the future.
Conclusions: We implemented a comprehensive lab stewardship program and piloted interventions to reduce unnecessary testing for 3 target tests. This process included establishing lab stewardship governance infrastructure, developing a framework to identify opportunities for safe reduction, and creating replicable processes to engage stakeholders, deliver educational content, deploy EHR modifications, and measure the impact of these interventions. This established infrastructure and successful pilot have created the foundation to assess impact and scale our program to identify and address additional opportunities to improve lab stewardship at our institution.