Background: The pediatric discharge education process currently struggles with a lack of standardization, miscommunication between care team members, and non-patient-centered discharge communication. These issues contribute to medical errors, increased readmissions, patient dissatisfaction, and unnecessary healthcare costs. The purpose of this study is to understand the current level of caregiver comprehension in our hospital, streamline the discharge process via process mapping, and thereby identify opportunities for improvement that have the potential to reduce miscommunication, errors, and preventable readmissions.
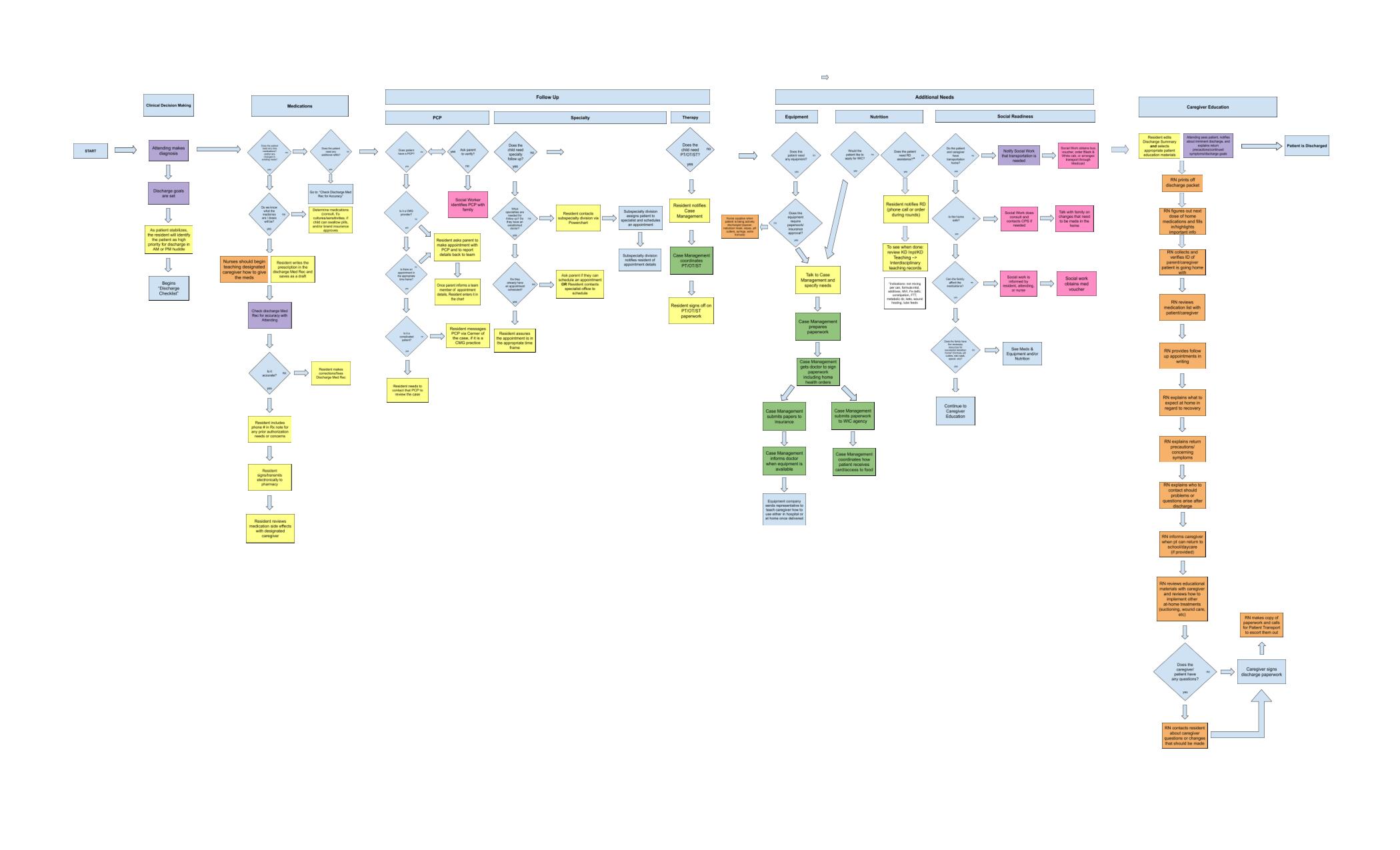
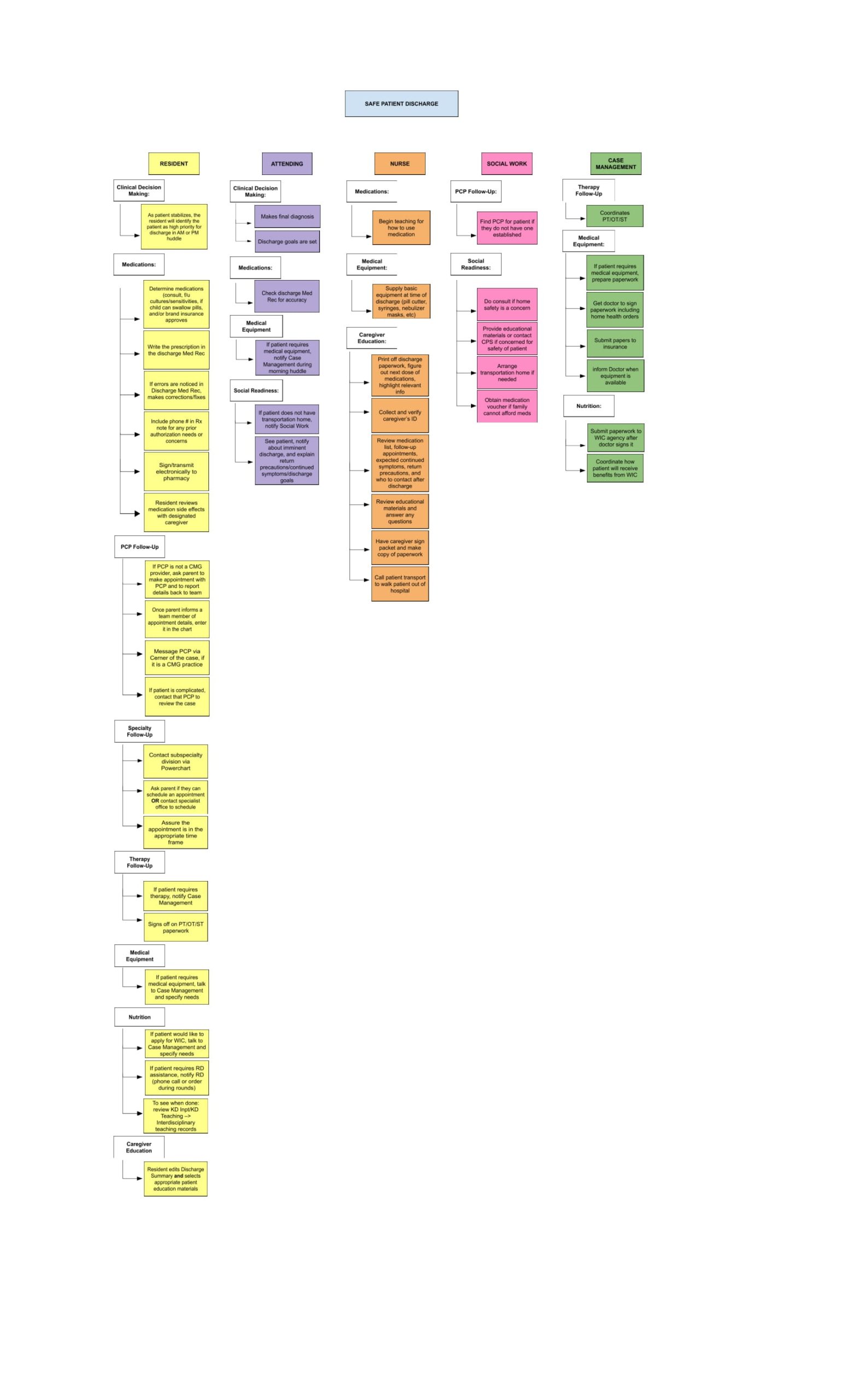
Methods: Summer research scholars attended interdisciplinary huddles and daily rounds with the healthcare team, observed discharge education provided by team members to families, and met with team members to formulate an understanding of the discharge process. The created process map was analyzed to identify any gaps with potential for improvement. Additionally, questionnaires were created to assess the caregiver’s comprehension of the discharge education, nurse prediction of the caregiver’s understanding, patient demographics, and revisit rates to the hospital or ER within seven days of discharge. Questionnaires were administered after education was completed. Caregiver responses were scored for accuracy, by comparison, to discharge education as documented in the patient’s chart. A 20% discrepancy between nurse prediction and the caregiver comprehension score was deemed a priori to be significant.
Results: The final process map consisted of over 75 steps, completed by six different healthcare provider roles. Summer research scholars identified over 20 discrete opportunities for improvement. These include making discharge criteria sets available to all the residents, starting the medical reconciliation during rounds and having the ability to draft it so that it can be crosschecked by an Attending Physician, and including a fax number and resident phone number on prescriptions for potential prior authorizations. Of the 93 patients whose education was reviewed, only 46% identified as non-white, but these accounted for 73% of the 15 cases in which a discrepancy in comprehension was identified. The return visit rate was 6.6%, with only 1 of these 6 having a greater than 20% discrepancy in comprehension scores.
Conclusions: Despite the relatively weak correlation between nurse prediction of caregiver understanding and patient readmission, several aspects of the discharge process were identified via process mapping that could improve patient understanding and reduce the likelihood of error, which could further ensure safe patient discharge and reduce readmissions. These include a need for functional improvements in the electronic medical record, better communication between members of the healthcare team, and increased team member role clarity.