Background: Given the rising demand for hospital-based providers, advanced practice providers (APPs; i.e., physician assistants/nurse practitioners) are increasingly being employed by hospitalist groups. However, APPs training in hospital medicine is variable and not always required. Post-graduate APP fellowships in hospital medicine have been previously described. However, fellowships are not widespread and data evaluating outcomes of APP fellowships remain limited.
Purpose: To evaluate APP fellowship graduates’ perceptions of the APP fellowship.
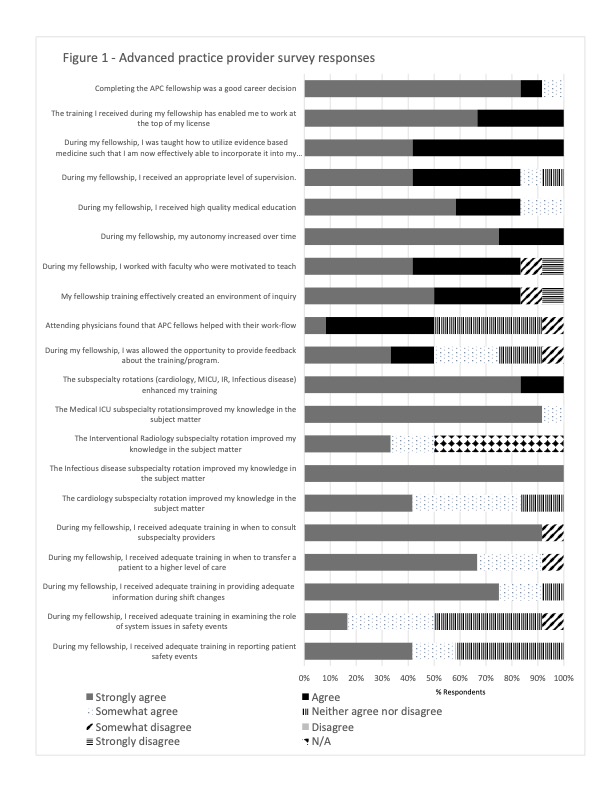
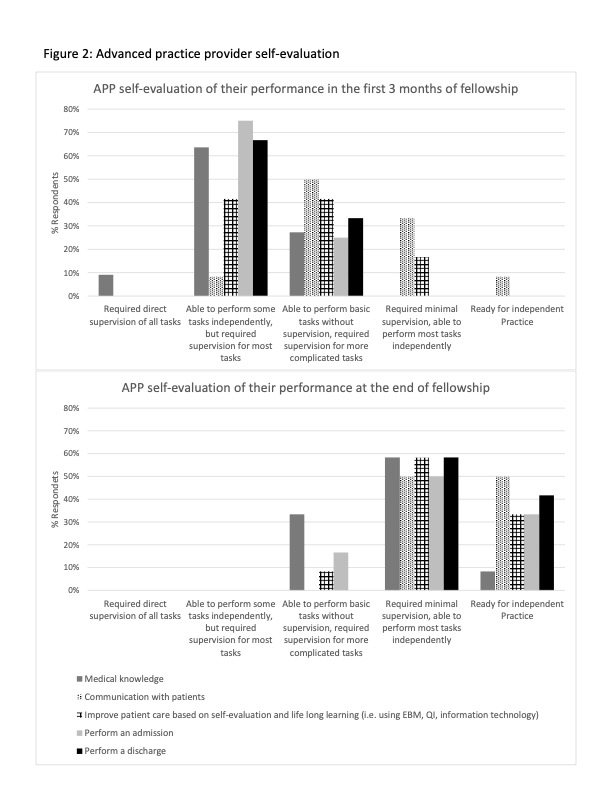
Description: We implemented an APP hospital medicine fellowship in 2017 within a large academic hospital. The 12-month fellowship consists of 9 months of hospital medicine and 3 months of inpatient subspecialty rotations. Clinical volumes for APP fellows are initially less than those of full time APPs and increase during the fellowship. Clinical work is supplemented by didactics, learning modules, and scholarly projects. We intend to offer successful graduates full-time APP hospitalist positions. Fellows are paid an annual salary ~30% less than full time APPs to support reduced patient loads, educational activities, and administrative costs of the fellowship.To better understand the impact of the fellowship on APPs, we surveyed 14 graduates of the fellowship regarding their experience (86% response rate, n=12). This study was approved by our IRB. Upon completion of the fellowship, 67% of APPs reported feeling comfortable caring for 7 or more complicated medical patients with little assistance. All APP respondents wanted to join our group “a lot” or “a great deal.” Other survey results are reported in Figure 1. APPs agreed or strongly agreed that the fellowship allowed them to work at the top of their license (100%), was a good career decision (93%), provided high-quality medical education (83%), had faculty who were willing to teach (83%), and created an effective environment of inquiry (83%). 75% of APPs said that program feedback was given on average every 3 months, and this was “neither too much or too little” (50%) or “slightly too little” (50%). After working with an attending, 75% of APPs said feedback was given most of the time or always. Figure 2 shows survey data of APP self-evaluation of their skills at the beginning of fellowship compared to the end of fellowship. By the end of fellowship greater than 80% of APPs thought they only required minimal supervision or were ready for independent practice in all tasks except medical knowledge (67%). At the end of their fellowship the percentage of APPs who were extremely comfortable or somewhat comfortable performing the following procedures were: ultrasound to assess fluid status 42%; performing thoracentesis 0%; performing paracentesis 50%; and performing lumbar punctures 16.7%.
Conclusions: Our findings suggest most APPs who completed a hospital medicine fellowship believed the fellowship was a valuable experience, was a good career decision, and that they received high-quality medical education. There was a strong desire to stay in the hospitalist group after the APPs graduated (86% [12/14] of graduates joined). Our survey demonstrated that our APP fellowship graduates welcome frequent feedback and that they do not feel adequately trained to perform bedside procedures. Future work is needed to determine if the fellowship leads to retention of APPs, to understand physician hospitalists’ perceptions of APP fellows, and the impact of the fellowship on patients’ clinical outcomes.