Background: Professional Advancement Models (PAM) have been researched and implemented at large academic institutions as a solution to provide structure and support for career advancement for Advancement Practice Providers (APPs).1,2 Many of these programs fail to appreciate the nuances of inpatient vs outpatient providers. Given the inherent differences of these practice settings, we aim to investigate the current state of professional development opportunities, interests and barriers encountered by inpatient and outpatient providers to inform the development of an institutional PAM program. To do this, we created and researched a hospital level needs assessment.
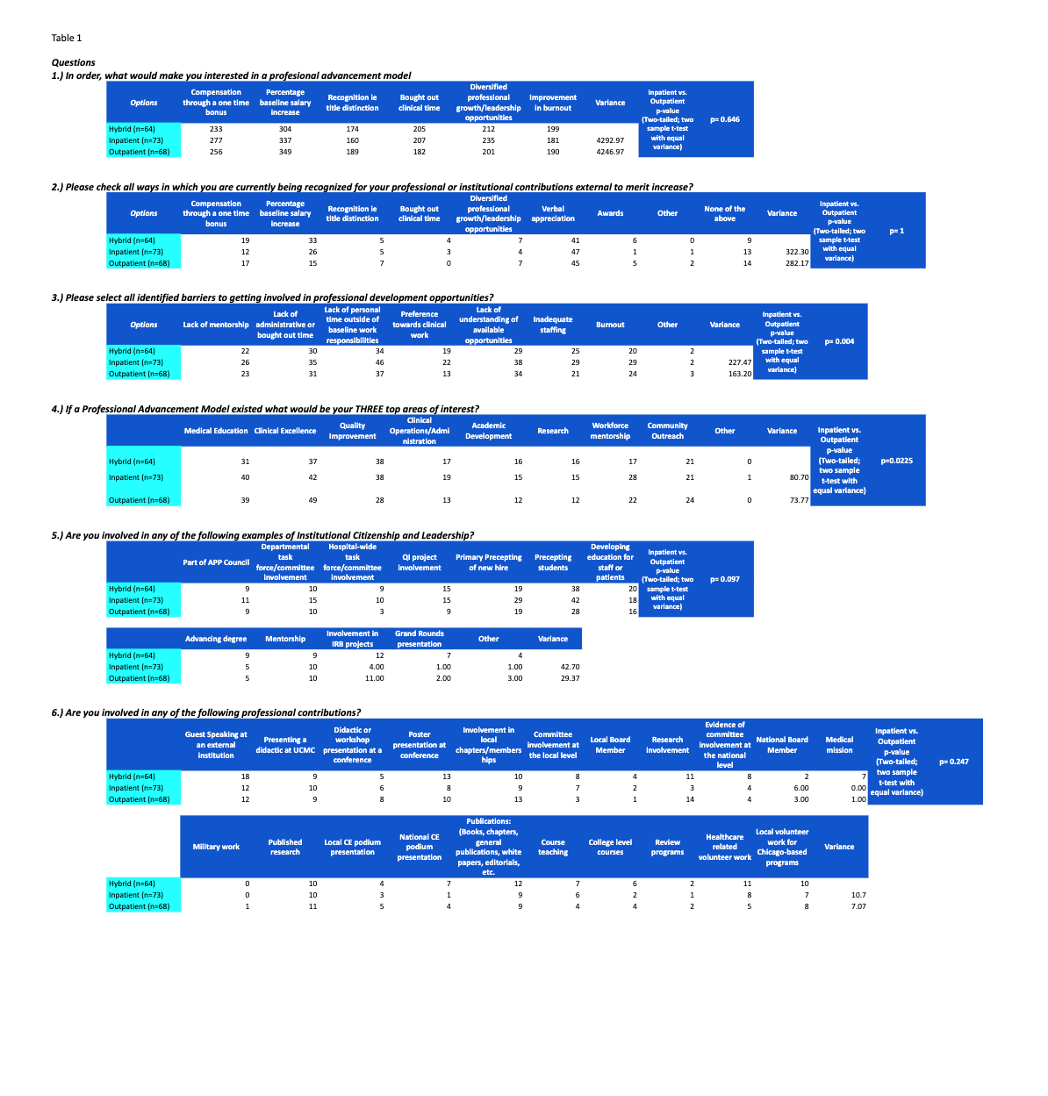
Methods: A survey was conducted where APPs identified inpatient, hybrid, or outpatient as their primary setting of employment, and answered 6 questions regarding professional advancement. 42% of all APPs in the institution responded (N=205) with 35.1% identified as inpatient (n=73), 34.2% as outpatient (n=68), and 30.7% as hybrid (n=64). A two-tailed, equal variance, two sample t-test was used to compare the total categorical and ranked responses per question from the inpatient APPs in comparison to the outpatient APPs. Hybrid responses were not considered for this comparison.
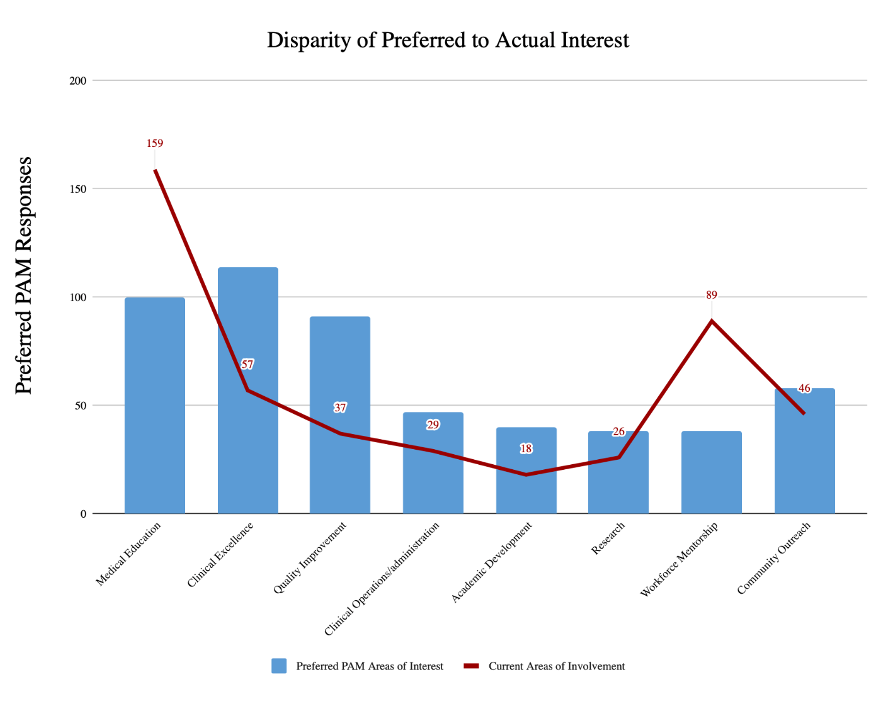
Results: Most questions did not reach statistically significant differences (p = < 0.05). Table 1 Question 3 found inpatient APPs to mark a greater number of barriers in comparison to the outpatient APPs (225:183; p = 00397). Questions 1 (p=0.65), 2 (p=1), 4 (p=0.225), 5 (p=0.097) and 6 (p=0.247) did not reach the defined threshold for statistical significance. Question 4, 5, and 6 were compared for rank. Without statistical significance of difference in the outpatient and inpatient group, both groups and the hybrid answers were collectively compared from question to question (N=205). Interests found a rank preference of clinical excellence (114), medical education (100), quality improvement (91), community outreach (58), Clinical operations (47), academic development (40), research (38) and workforce mentorship (38). Current areas of involvement found a rank of medical education (159), workforce mentorship (89), clinical excellence (57), community outreach (46), quality improvement (37), clinical excellence (29), research (26), and academic development (18). Figure 1
Conclusions: Barriers to professional development were cited to a greater degree by inpatient both in total and for each option individually. This warrants further evaluation into why discrepancies exist. However, since the experiences of both groups have similar recognition modalities, areas of interest, and areas of current and previous involvement, a standardized PAM program for both parties can be developed. As a PAM program is created, it is important to note the areas of interests are not aligned with the areas of current involvement for APPs across settings, suggesting disparity in opportunities. This could identify a need for the PAM to increase focus and program development in the areas of interest of APPs to improve professional satisfaction specifically in clinical excellence, medical education, and quality improvement. In next steps, the PAM taskforce will utilize lessons learned from the needs assessment to develop a business proposal that will be presented to stakeholders to garner support and input on the program.