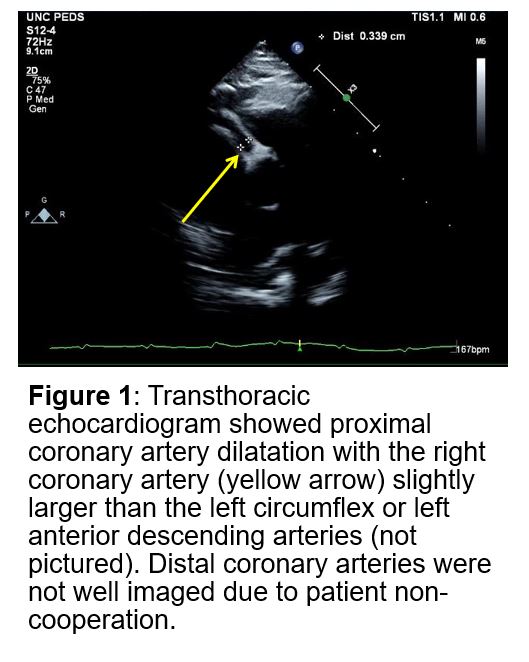
Case Presentation: A 5-month-old male presented to the hospital for further workup of 15 days of fever. In the preceding 2 weeks, he had intermittent symptoms, including cough, rhinorrhea, and diarrhea. He was treated for an ear infection with antibiotics about 5 days into the course for suspected otitis media without resolution of his fever. He subsequently developed a transient erythematous rash on his abdomen, back, and lower extremities thought to be due to the antibiotics. The rash resolved prior to presentation. In the emergency room, labs revealed pancytopenia and he was admitted due to concern for malignancy. On exam, the infant was very well-appearing with normal vitals other than persistently elevated temperatures. Labs showed pancytopenia (Hb 6.6g/dl, platelets 37×10*9/L, WBC 6.3×10*9/L, ANC 1000×10*9/L), albumin 2.6mg/dl, AST 85u/L, ALT 119u/L, normal alkaline phosphatase and bilirubin, and urinalysis with sterile pyuria. Flow cytometry and peripheral smear were not consistent with leukemia. He continued to have daily fevers despite antibiotics and supportive care. He had no oral lesions or erythematous tongue, lymphadenopathy, extremity changes, or conjunctivitis. Infectious workup for bacterial, fungal, and viral pathogens was negative. Additional studies revealed fibrinogen 241mg/dl, CRP 54mg/dl, ESR 44mm/h, ferritin 322ng/ml, D-dimer 835ng/ml, triglycerides 449mg/d. An echocardiogram on day 3 showed diffuse dilatation of the proximal coronary arteries. The patient was diagnosed with incomplete Kawasaki disease and treated with intravenous immunoglobulin (IVIg), aspirin, and prednisolone. His fevers resolved upon IVIg treatment and he was discharged home on prednisolone and aspirin. Repeat echocardiogram 2 months later showed stable coronary artery dilatation.
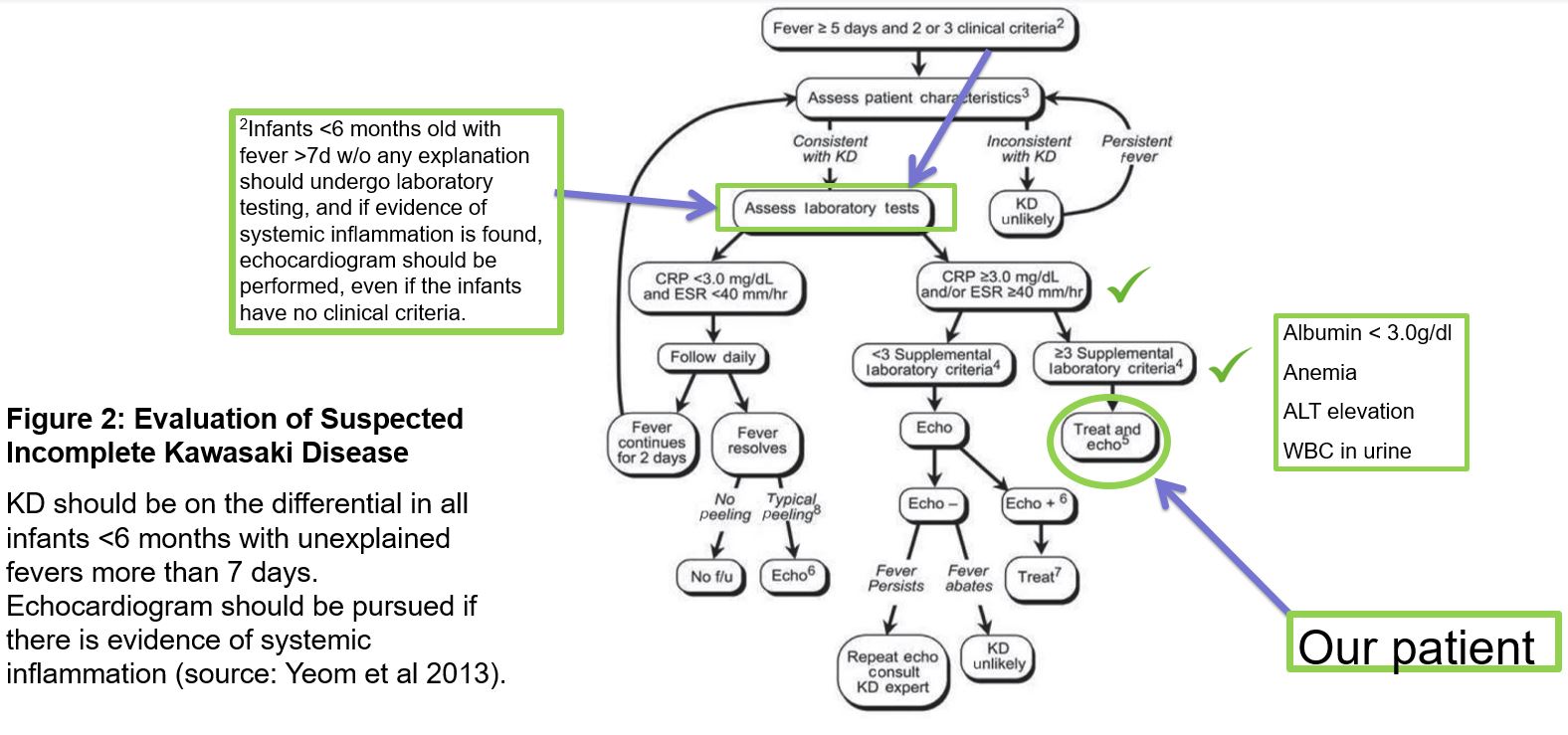
Discussion: Kawasaki disease (KD) is a systemic vasculitis most commonly seen in the setting of conjunctivitis, mucositis, rash, and lymphadenopathy, however not all children present meeting the classical diagnostic criteria. This is particularly true in infants. Our patient met incomplete criteria with elevated inflammatory markers, elevated ALT, sterile pyuria, and hypoalbuminemia. Early diagnosis is important so treatment with IVIg can be initiated to prevent coronary artery aneurysms, a hallmark of the disease. Studies show that infants (particularly less than 6 months old) take the longest time to diagnose and are least likely to fulfill diagnostic criteria. As a result, they are at highest risk for developing coronary artery abnormalities. Diagnosis was delayed in our patient because of the atypical presentation, but also because of his blood cell abnormalities. Typically, white blood cells and platelets are elevated in KD – our patient presented with pancytopenia which initially raised significant concern for leukemia. Once malignancy was ruled out, additional testing resulted in the diagnosis. Because of the difficulty in making this diagnosis in infants, some studies advise echocardiogram in this age group if there is evidence of systemic inflammation, even without clinical criteria.
Conclusions: Infants are more likely than other age groups to present with atypical features of Kawasaki disease, and as a result, diagnosis is often delayed. It is important to have a high clinical suspicion in infants with fever of unknown origin and consider KD early to initiate treatment and prevent coronary artery pathology. While unusual, pancytopenia has been reported in other cases of Kawasaki disease.