Background: Atrial fibrillation (AF) is strongly age-dependent, and with a growing geriatric population, the incidence and prevalence of AF is expected to increase in the United States. As a result, the number of patients at risk of a thromboembolic event due to AF is also expected to increase. Although bleeding associated with mechanical falls is a major reason preventing an elderly patient from being on anticoagulation, the patient would have to fall 300 times/year for the risk of bleeding complications from falling to outweigh the benefits of prevention of thromboembolic stroke. Using data from a large health system, we examined the predictors of anticoagulation prescription during discharge in elderly patients with AF after in-hospital fall.
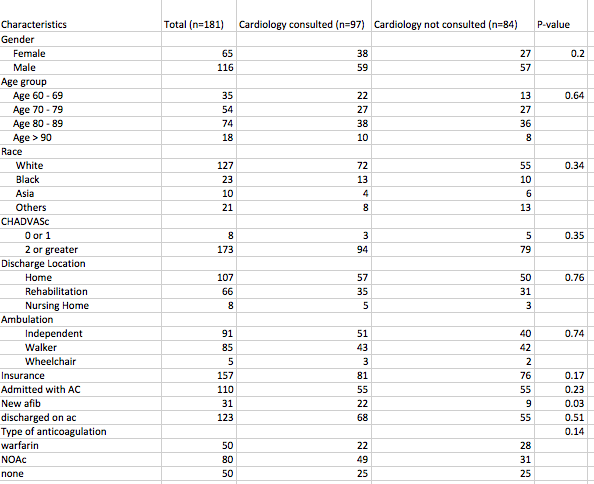
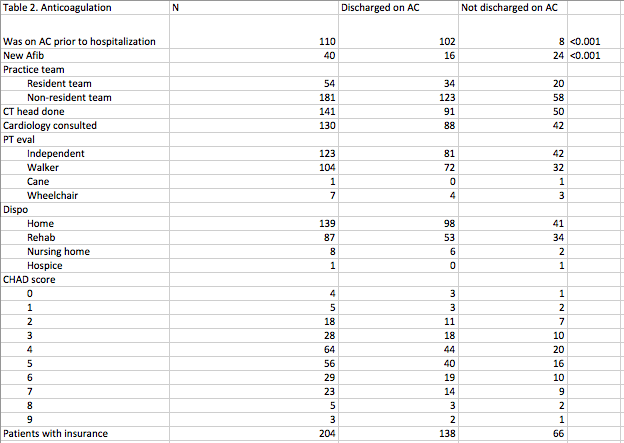
Methods: We included patients 60 years and above discharged from 2013 to 2018 with a diagnosis of AF and a secondary diagnosis of in-hospital fall during that admission. We excluded patients with subarachnoid hemorrhage, gastrointestinal bleeding or other contraindications to anticoagulation. We described demographics including race/ethnicity, gender, age group (60-69, 70-79, 80-89, 90+), and insurance status. We also examined clinical characteristics including being on a resident team, cardiology consult, CT head performed after the fall, ambulation status (independent, walker, or wheelchair), discharge location after physical therapy evaluation (home, rehab, or nursing home) and calculated CHA2DS2-VASc score for each patient. The primary outcome was prescription of anticoagulation during discharge. We first stratified the study sample by whether or not patients received a cardiology consult during hospitalization and then by anticoagulation prescription upon discharge. Among patients with a diagnosis of AF, we ran multivariable logistic regressions to identify predictors of anticoagulation prescription upon discharge.
Results: A total of 181 patients met the study criteria. The population was 70% white, 52% ambulate independently, 87% were insured, 96% had a CHA2DS2-VASc score greater than or equal to 2, and 17% had new AF during that admission. There was no difference in cardiology consultations called or head CT performed by demographics characteristics, but higher percentage of patients with new AF received a cardiology consult (p=0.03). A higher percentage of patients taking anticoagulation on admission was prescribed anticoagulation on discharge (P<0.001), while a smaller percentage of patients with new-onset AF was prescribed anticoagulation on discharge ((P<0.001). Among patients with existing diagnosis of AF, being on anticoagulation prior to admission increased the odds (Odds ratio=127.33 [25.31-640.55]) of being discharged home with anticoagulation and Asians were less likely to be discharged on anticoagulation (Odds ratio=0.05 [95% CI 0.00-0.45]).
Conclusions: Our findings show that elderly patients with a diagnosis of AF who are on anticoagulation before admission are more likely to be discharged on anticoagulation after a fall. In elderly patients with a new diagnosis of AF, having a fall significantly decreased the odds of being prescribed anticoagulation on discharge. These results suggest that providers’ decisions on anticoagulation in the elderly with new diagnosis of AF and fall seem to be guided more by their concerns over bleeding complications than by the patient’s risk for stroke, suggesting that anchoring bias may benefit patients with AF on anticoagulation who fell in-hospital.