Background: Although Hospice has been associated with improved symptom management, quality of life, lower costs and length of survival in terminally ill patients, it is underutilized. The primary outcome of this study was to examine the relationship between hospice enrollment status and hospital readmissions in elderly patients with solid tumors. Secondary outcomes were length of stay, ICU admissions, mortality, code status, LACE scores and frequency of geriatric and palliative care (GAP) consults and palliative care unit admissions.
Methods: This was a retrospective cohort study on patients older than 65 years old with solid tumors admitted to a tertiary hospital (12/1/12-3/1/15). Patients were divided between those enrolled in hospice and those not enrolled but with criteria suggesting hospice eligibility (Metastatic disease and Karnofsky Performance < 50%). Descriptive statistics were calculated with two sample t-tests for continuous measures and odds ratio for secondary outcomes using SAS 9.4
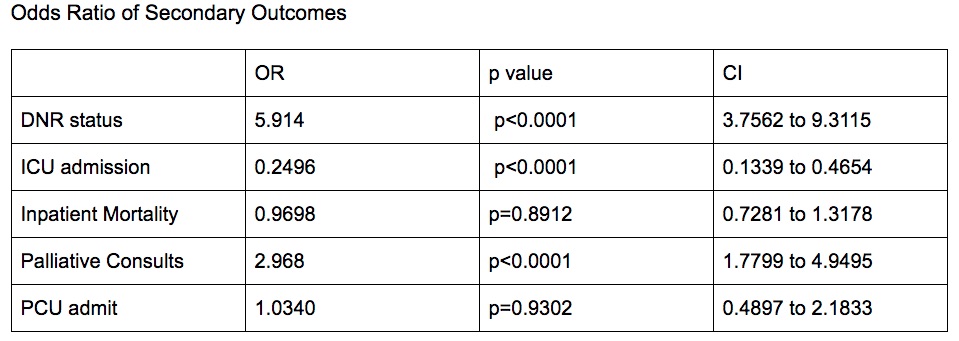
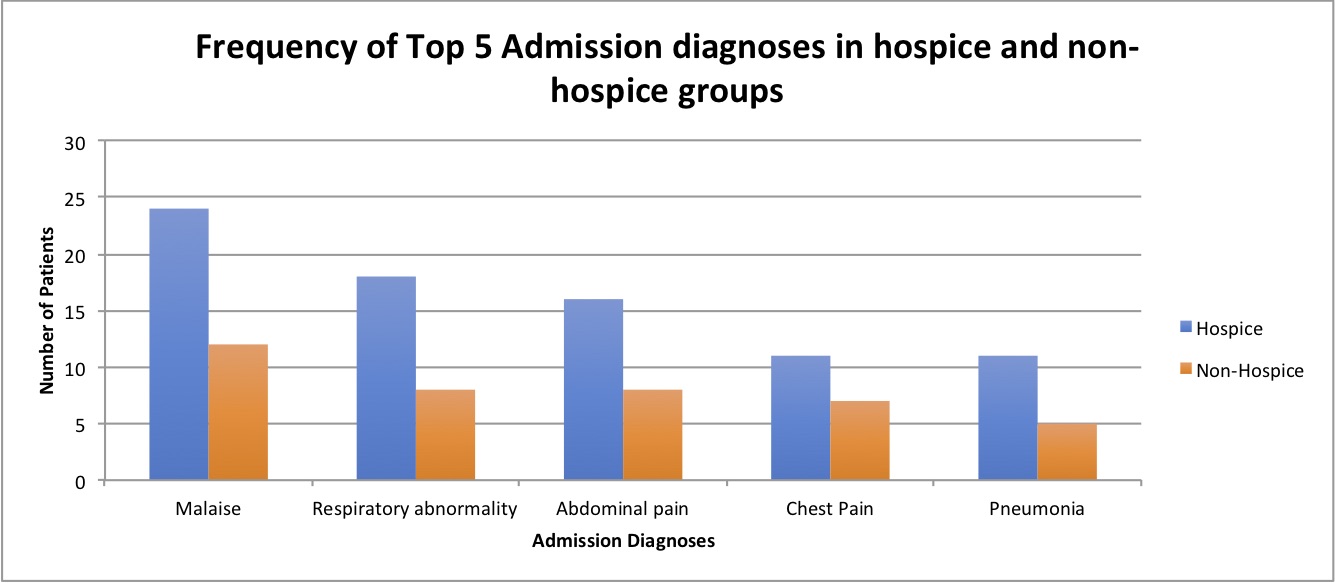
Results: A total of 382 patients were analyzed and the hospice and non-hospice groups showed comparable similarities on their demographics and Charlson scores (p=0.644). There was higher readmissions in the non-hospice group (30.5%, mean=0.760, SD=2.1) than hospice group (36%, mean=0.402, SD=0.573), p=0.0064 and higher LACE scores with (mean=10.2, SD=2.09) than hospice group (mean=9.80, SD=3.17), p=0.0175. There was no significant difference in LOS between the two groups. Both the odds of DNR (5.91) and the odds being seen by palliative (2.97) is more in the hospice group than the non-hospice group both at p<0.0001. The odds of of ICU admissions in the hospice group are 0.25 lower than in the non-hospice group at p<0.0001. The odds were not significant in hospital mortality or palliative care unit admissions between hospice and non-hospice groups. The top admission diagnoses in both hospice (10.2%) and non-hospice groups (8.2%) were malaise.
Conclusions: Elderly patients with solid tumors that may be eligible for hospice services, if not identified, may be prone to frequent readmissions and aggressive interventions. GAP consultation may further help with identifying this vulnerable population in order to improve their outcomes. However, more research is needed to closely study the effects of hospice in reducing hospital complications and where these benefits may further help