Background: Existing research describe older adults’ sub-optimal experiences of the hospital to skilled nursing facility (SNF) transition. However, these studies do not explore the causes of these poor experiences and neglect the complex clinical system in which these transitions occur. Therefore, the aims of this study were to identify the causes of patient experiences during the hospital to SNF transition.
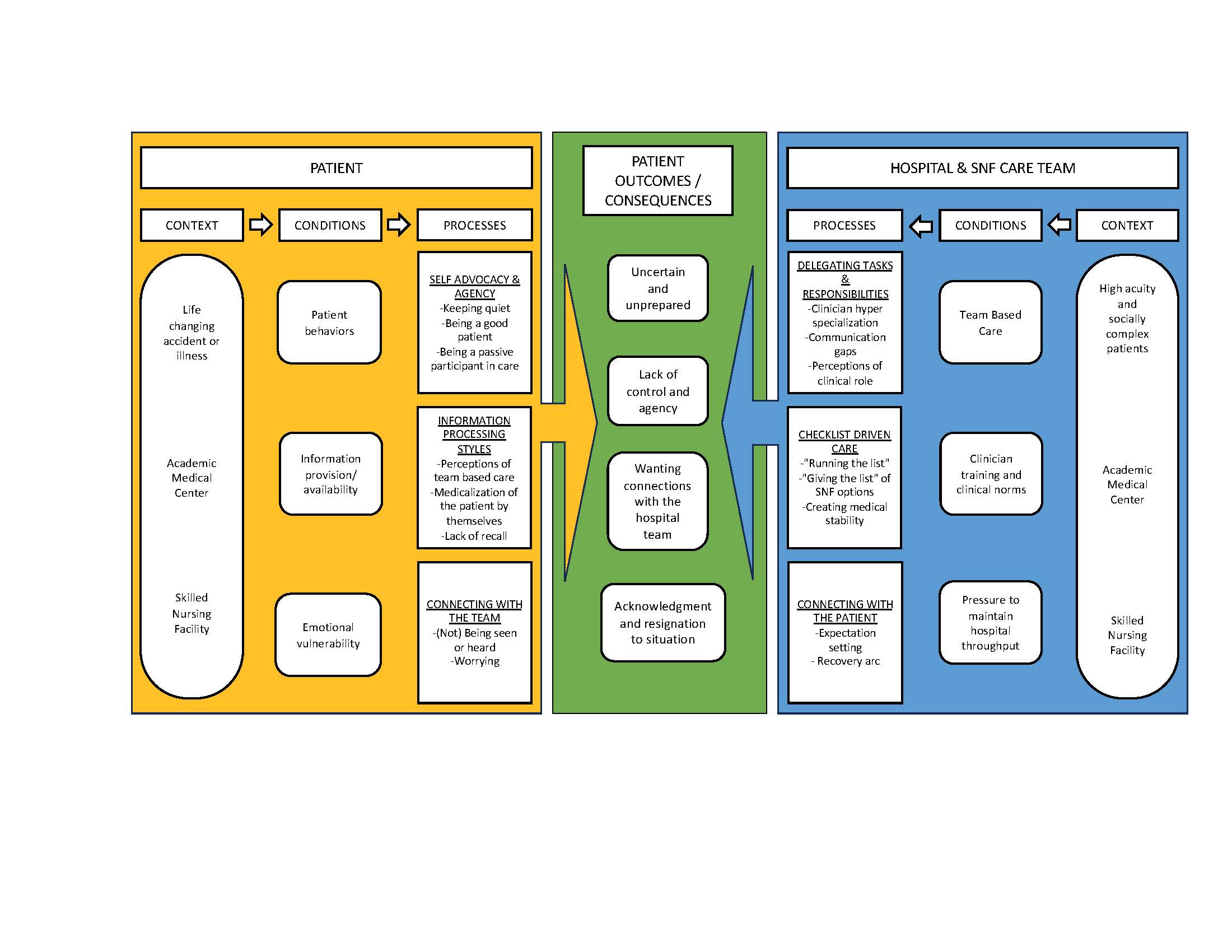
Methods: We conducted a grounded theory qualitative study. This study took place on the Medicine Service at an urban academic medical center (AMC) and urban short-term rehabilitation SNF. Patients were eligible if they were ≥65 years old, English speaking without dementia. Patient caregivers, AMC and SNF clinicians were also eligible. We conducted individual in-depth interviews with patients, caregivers, and clinicians; and ethnographic observations of care activities (e.g., rounds, family meetings, discharge planning and SNF admission). We used dimensional analysis to analyze data. Dimensional analysis involves creating an explanatory matrix of prominent dimensions that consider the context, conditions and processes that result in specific consequences or outcomes.
Results: We completed 41 interviews (16 patients, 4 caregiver and 25 clinicians) and 30 hours of ethnographic observations. There were four major patient outcomes: feeling uncertain and unprepared about the SNF admission; a lack of control and agency; a desire for better connections with the hospital team; and an acknowledgement and resignation to their current situation and realities of a fragmented healthcare system (Figure 1). Dimensions causing these outcomes were a result of patient and care team factors. Patient behaviors such as taking a passive role in their healthcare impacted their recall, understanding and agency. Patients often focused exclusively on information provided by physicians rather than other members of the care team. Patients’ emotional vulnerability exacerbated their desire to be seen and heard by the care team. Clinicians’ perceptions of their professional role led to delegation of clinical tasks and responsibilities. This resulted in tasks related to patient engagement and communication being overlooked or assumptions that these tasks were completed by someone else. Clinical practice and training focus on checklists and standardized care processes, but these checklists often omitted counseling patients about what was important to them about SNFs and their recovery. The care team’s ability to spend time with patients was hindered by a pressure to maintain hospital throughput.
Conclusions: The causes of patients’ sub-optimal hospital to SNF transition are multifactorial related to patient behaviors, how patient’s process information and their emotional state as well as clinical practice styles and processes. Improving this transition will require targeting patient, care team, and health system factors in combination to have maximal effect.