Background: There are over 35 million discharges from inpatient hospitalizations annually in the US. During these transitions of care, patients are at risk for adverse events. It is crucial for patient safety to have accurate communication between the inpatient physician and the provider assuming care.The main conduit for this communication is the hospital discharge summary. In a recent national survey, 94% of primary care providers (PCP’s) identified an accurate medication list as the most important component of a discharge summary (1). However, medication discrepancies are among the most common errors in discharge documentation and occur in up to 71% of discharge summaries (2).At our institution we noted that many of our discharge summaries did not have accurate medication lists. We aimed to develop a quality improvement project to improve the accuracy. In this study we analyzed pre-intervention data.
Methods: We performed a single-center retrospective observational cohort study of all adult patients discharged from the internal medicine service at an academic hospital between December 1, 2021 – December 1, 2022. Patients were assigned to one of two cohorts, those with a reconciled medication list on their discharge summary versus those without a reconciled list. Our objective was to compare clinical outcomes between these cohorts. The primary outcome was 30-day hospital readmission. Secondary outcomes included 7- and 30-day post-discharge ER visits, clinic visits, and mortality.A text search tool was used to search discharge summaries for the standardized term “medications NOT reviewed” which indicated an unreconciled medication list. Study outcomes were compared using the Chi-squared test. A p-value of 0.05 was used to determine significance. Stata/IC 16.1 (Statacorp College Station, Texas) was used to perform the analysis.We excluded patients discharged as deceased or to inpatient hospice, and discharge summaries not signed by an internal medicine physician. We reviewed duplicate discharge summaries and excluded the earliest summary. We excluded 84 summaries, and the final data analysis included 8653 discharge summaries.This study was determined to be exempt by the IRB.
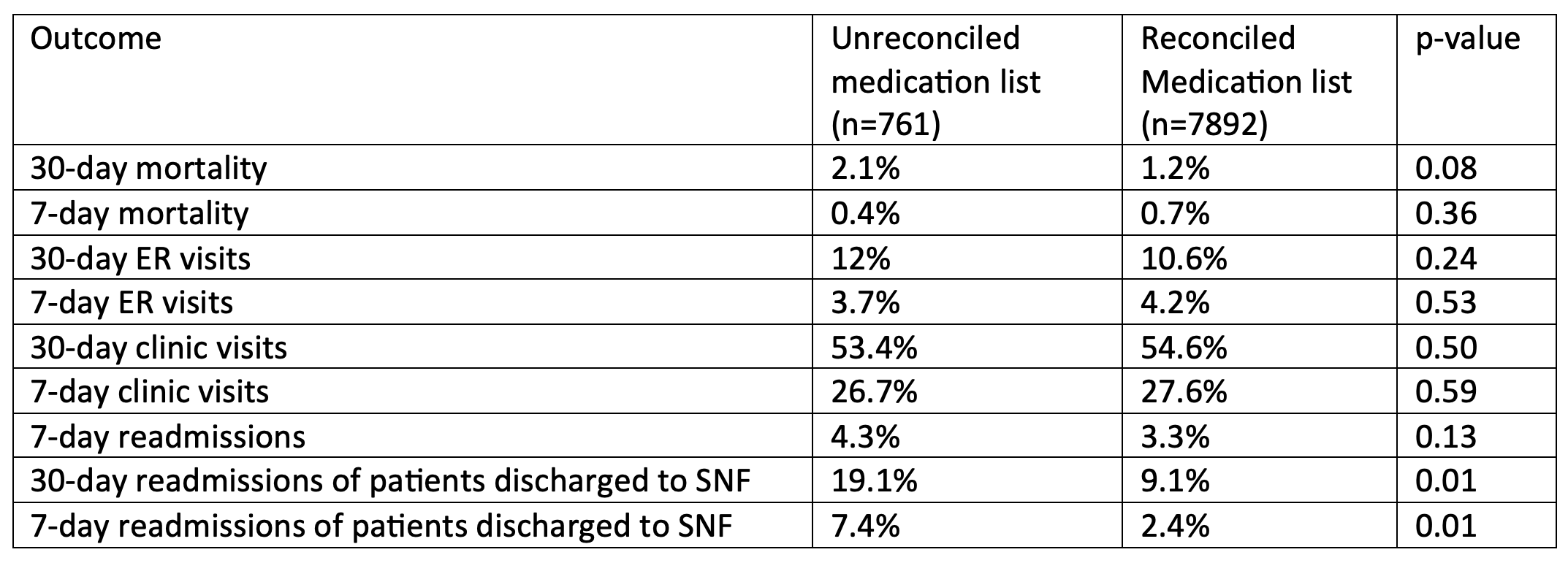
Results: There were 761 (8.8%) discharge summaries with an unreconciled medication list, and 7892 discharge summaries with a reconciled list. In the unreconciled medication list cohort, 30-day hospital readmissions were 12.8% versus 10.8% in the reconciled list cohort (p = 0.10). Apart from a subgroup analysis examining readmissions among patients discharged to a skilled nursing facility (SNF), there were no statistically significant differences in secondary outcomes (Table 1).
Conclusions: In our study 9% of discharge summaries did not have an accurate medication list. Although we did not observe significant differences in study outcomes, we believe accurate medication lists are important for transitions of care following hospital discharge. PCPs identify accurate medication lists as an important component of a discharge summary. Interestingly, subgroup analyses show a statistically significant increase in both 7- and 30-day readmissions for patients who were discharged to a SNF and had an unreconciled medication list on their discharge summary. The cause of this association is unclear but may be explained by SNF providers relying more heavily on the discharge documents compared to other providers. We plan to institute an EMR-based quality improvement project to improve the accuracy of discharge medication lists.