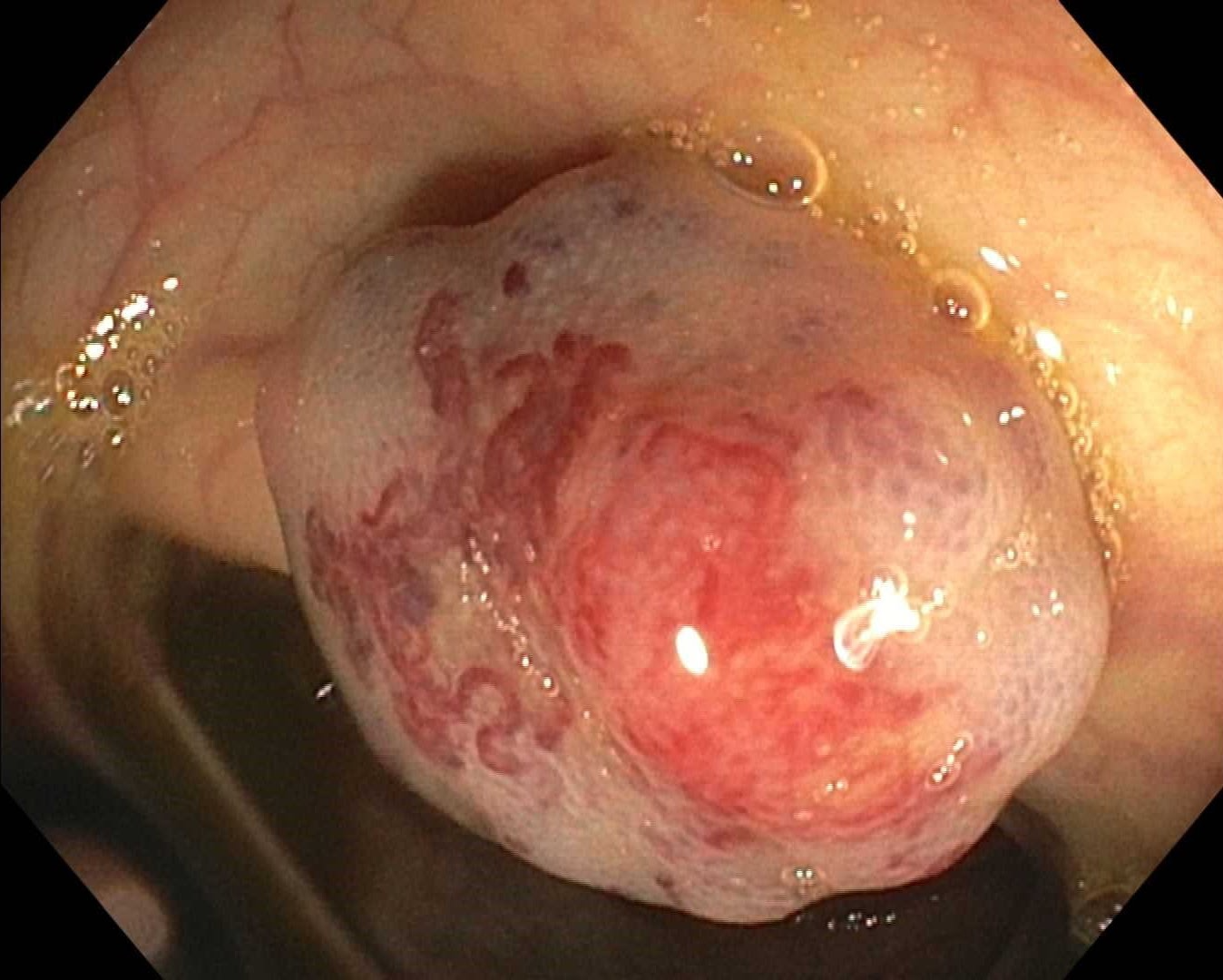
Case Presentation: This patient is a 34 year old female presenting to the ED complaining of progressive weakness,SOB, bloody vomitus, and tarry stool. She had PMH significant for established diagnosis of Bean Syndrome. On presentation she was normotensive, 113/72mmHg but tachycardic 102. Labs revealed acute microcytic anemia H/H 6.7/23.6 MVC 70.9 prior to transfusion. She was transfused a total of 4 units pRBC with H/H improving to 10.8/37.3. On physical examination the patient had multiple scattered blebs including the toe, neck, torso, and buttock. Periumbilical tenderness was noted with localization to RU/LQ prompting abdominal US demonstrating multiple cystic hepatic lesions. Further investigations including abdominal MRI were completed with T2 bright/T1 dark, nonenhancing foci appreciated, clues pointing towards venous malformations. In light of patients’ established diagnosis and acute anemia, gastroenterology was consulted.
Discussion: BRBNS is a sporadically inherited disorder caused by mutations in the TEK gene encoding for TIE2; leading to multifocal hemangiomas due to two activating mutations. These make diagnosis difficult to distinguish from comparatively more common conditions such as Maffucci’s with soft vascular lesions overlapping with the bony enchondromas; or Kippel-Trenaunay-Weber with characteristic capillary-lymphatic-venous malformations and associated bony hypertrophy. Areas of particular overlap between the two: d-dimer elevation and lesion distribution; GI tract involvement in KTW (colon), and in BRBNs (small intestine). D-dimer elevation while a nonspecific finding is linked to diffuse multifocal VM, associated with an increase in size and number of lesions, particularly with base-line d-dimer elevation >0.5mg/L, such as our patient with D-Dimer at 1.53. Beans can occur at any age but most commonly appears in adolescence, 55% presenting before the age of 18, such as our patient diagnosed at the age of 12. Her presentation encompassed a variety of manifestations reported previously in literature, but also highlighted distinctive features. The absence of duodenal involvement was notable, and drew attention to the various anomalies a patient can present with in this disease. Highlighting this disease and reporting it with all available comparative data is the key in raising awareness, improving recognition, diagnosing early, and effectively treating.
Conclusions: Medical treatment for this condition is early in its trial period and includes- Octreotide: functions by decreasing splanchnic blood flowSteroids/Interferon alpha: Anti-angiogenic effect in controlled trialsSirolimus: mTOR pathway inhibitor. Surgical treatment options involve resection, band ligation, and endoscopic cauterization, successful outcomes reported in bleeding episodes that are recurrent or severe. Due to the rarity of Blue Rubber Bleb Nevus Syndrome, it is vital for research to highlight patient cases of atypical presentation to educate the medical community and ultimately improve patient management and outcomes. The disease itself is novel and treatment therapies are in their early phase of study. Through recognition of patient encounters, treatment trials, and case reporting we hope to bring light to Blue Rubber Bleb Nevus Syndrome and pique the interest of our audience. Medicine is a truly vast and endless field, encounters such as these that arouse our curiosity and cause us to dig a little deeper into our everyday practice help shape ourselves as better physicians for the future.