Background: Patients in hospitals often face various physical constraints, such as being monitored, having internal or external catheters inserted, or being tethered to an IV pole. These limitations act as barriers to mobilization, contributing to the deconditioning of patients who initially mobilized independently or with assistance, leading to increased falls, excessive use of physical therapy resources, and a rise in patients requiring sub-acute rehabilitation facilities instead of returning home.
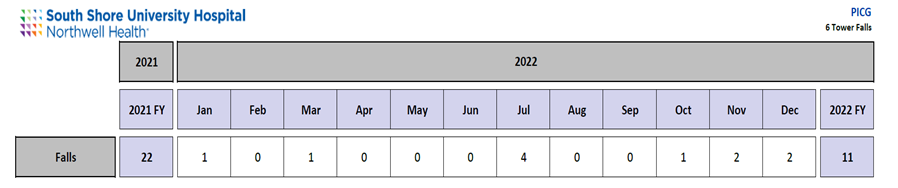
Purpose: The goal is to promote mobilization, decrease patient deconditioning, minimize falls, and concurrently reduce the overreliance on physical therapy consultations.
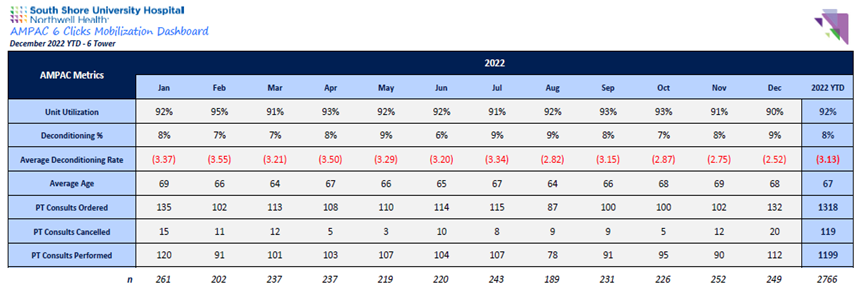
Description: Our organization prioritized mobilizing patients, starting with encouraging them to be out of bed for meals. A scripted approach was developed to emphasize the importance of mobilization as part of the daily healing process. The nursing staff on a medical/surgical unit received education on an objective tool, AMPAC 6 clicks (Activity Measure for Post-Acute Care), used to assess functional status. This tool was integrated into daily interdisciplinary rounds, and the daily functional assessment score was reported. Physical therapy and the providers on rounds re-educated nursing on interpreting the score and addressing patient needs. Physical therapy consults were canceled based on these discussions. Nursing leadership ensured nurse accountability for patient mobilization through audits. Devices such as telemetry, continuous pulse oximeters, and catheters were removed to eliminate physical barriers to mobility.
Conclusions: The nursing utilization of AMPAC 6 clicks exceeded 95% on this unit in 2022, covering over 2,766 patients. Despite 1,199 physical therapy consults conducted, this initiative resulted in the cancellation of over 119 consults within a year. There was a notable reduction in falls from 22 in 2021 to 11 in 2022, along with a significant decline in sub-acute rehab referrals. Overall, optimizing mobility led to improved quality outcomes.