Background: Although hip fractures in the elderly are largely due to osteoporosis, rates of treatment for osteoporosis after fragility fracture have been reported as <10%.1 Our hospitalist group cares for all hip fracture patients at our institution but had no process for evaluating or referring patients for osteoporosis treatment. Our objectives were 1) To determine baseline rate of evaluation and treatment for osteoporosis among hip fracture patients treated by UNC Hospital Medicine and 2) To determine impact of a new referral process on rates of evaluation and treatment.
Methods: Baseline data were obtained by query of electronic medical records (EMR) for inpatient visits to UNC Hospital Medicine with International Classification of Diseases, version 10, codes S72.x, as a primary or secondary diagnosis, over the academic year July 2018 – June 2019. Patients <50 years and those with high-energy trauma or pathologic fracture were excluded.Our intervention included institution of endocrinology consultation for all patients with acute hip fracture, beginning July 2019.Outcomes included rates of diagnosis of and evaluation for osteoporosis at the time of hospital discharge and rates of diagnosis, evaluation and treatment within three months of discharge, before and after intervention. Definitions were as follows: Diagnosis – any listing of osteoporosis in discharge summary, clinic note or problem list in EMR Evaluation - any one of following: - Endocrinology consultation or referral - DEXA scan - Documented plan for treatment in EMR Treatment - Initiation of meds if treatment naïve OR - Intensification of meds if on treatmentThree-month outcomes were recorded only for patients with a primary or specialty physician from our institution or with outside primary care notes visible in our EMR.
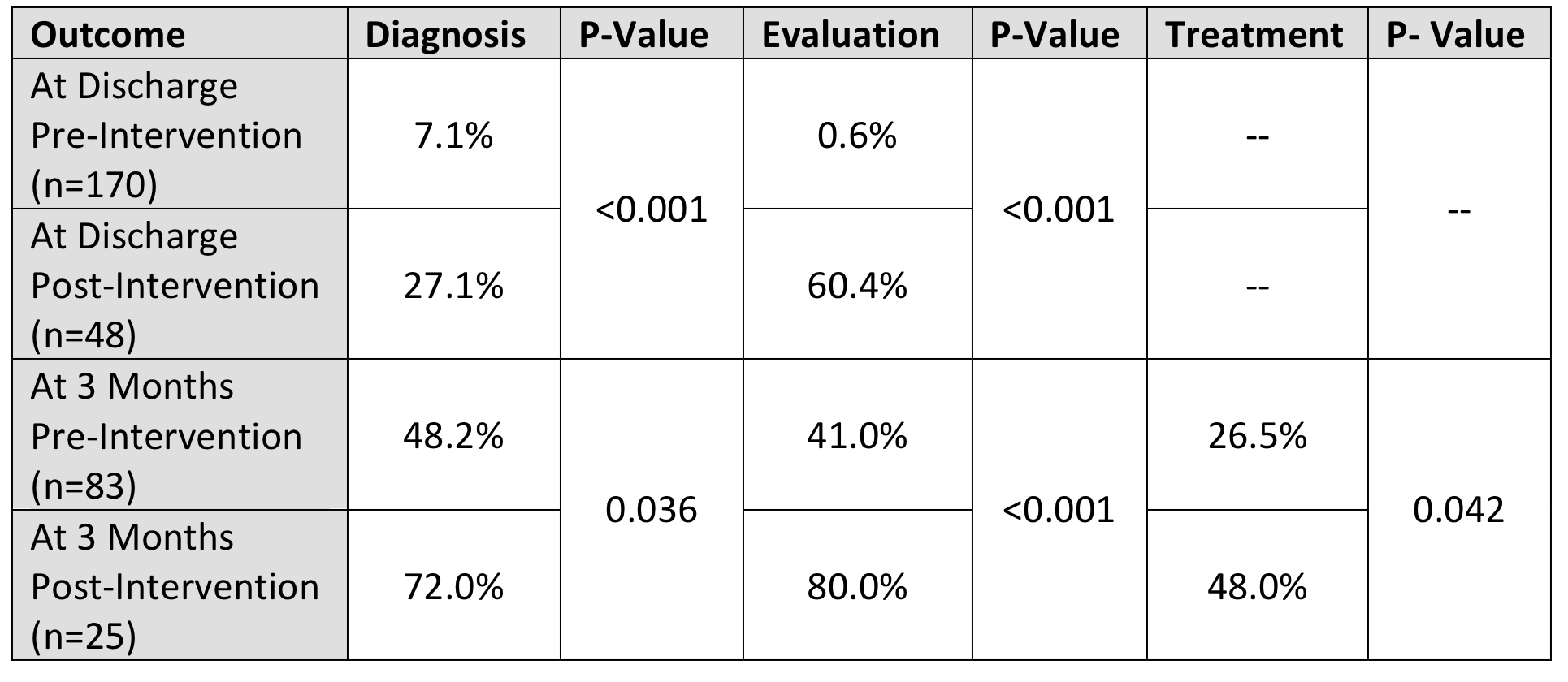
Results: We identified 170 patients hospitalized with hip fracture before and 48 patients after our intervention. Among pre-intervention patients, mean age was 80 years, 76.3% were female, 87% were white, and the mean length of stay was 5.5 days and there were no statistically significant differences between pre- and post-intervention populations. Outcomes are summarized in Table 1, with significant improvements noted in all measures.
Conclusions: Among patients hospitalized by UNC Hospital Medicine for fragility hip fracture before our intervention, few had a documented diagnosis of osteoporosis and almost none were evaluated for osteoporosis by the time of discharge. Within three months of discharge, fewer than half of patients were evaluated and only a quarter were treated for osteoporosis. Post-intervention rates of diagnosis, evaluation and treatment were all significantly improved,with almost half of patients being treated within three months of discharge. Inpatient endocrinology consultation for patients with fragility hip fracture correlated with statistically and clinically significant improvements in subsequent evaluation and treatment of osteoporosis.