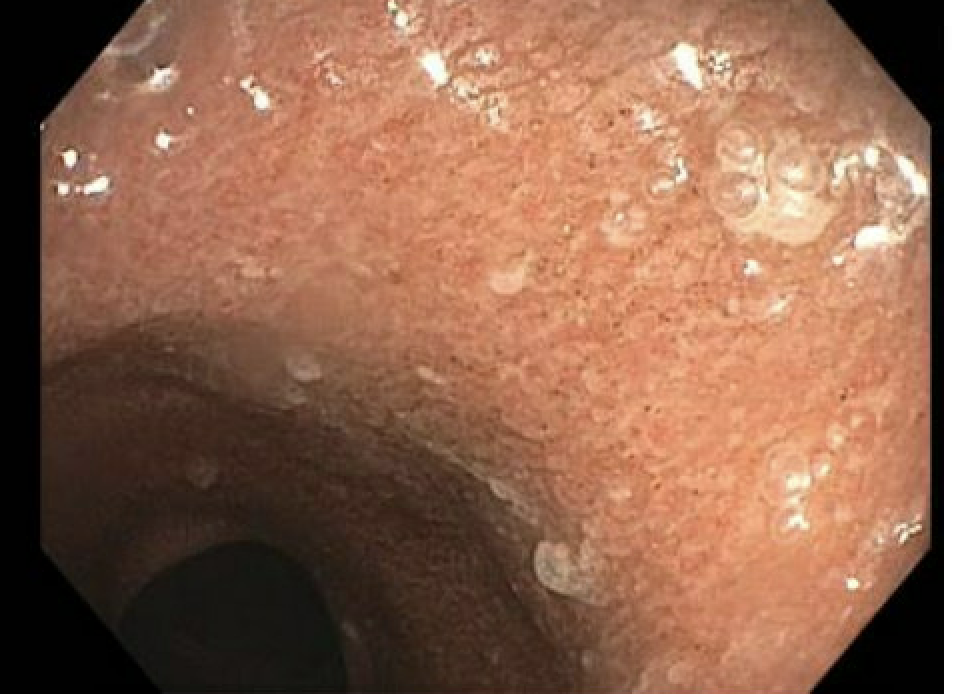
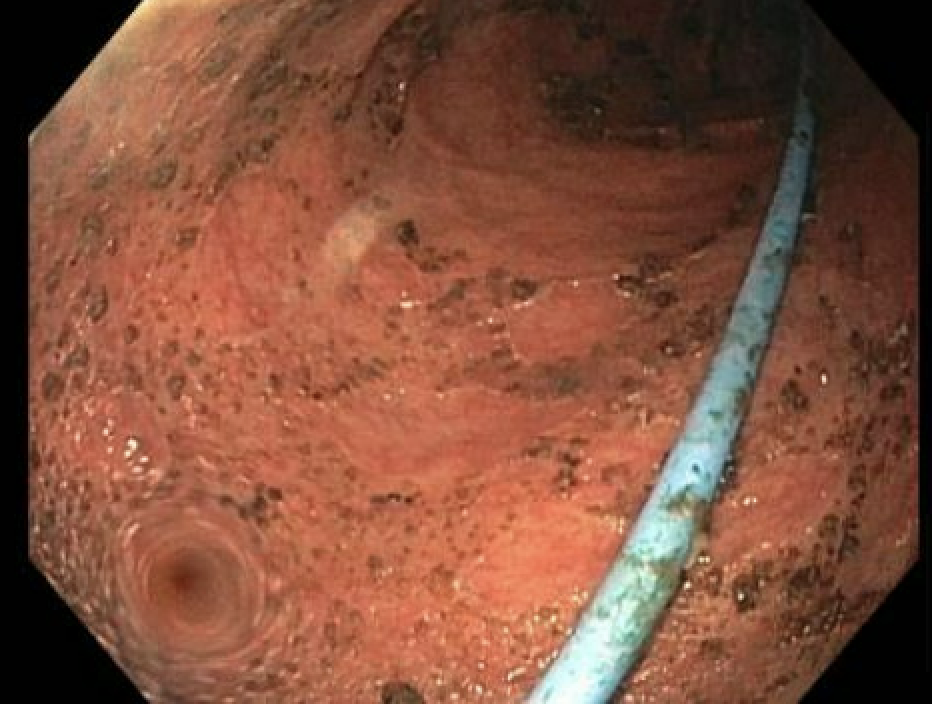
Case Presentation: An 80-year-old male with a history of collagenous colitis, hypertension, type 2 diabetes, microcytic anemia, exocrine pancreatic insufficiency, severe malnutrition, and vitamin D deficiency presented with weakness, chronic diarrhea, and significant weight loss (~100 lbs in one year). He had 5-7 non-bloody stools daily, unresponsive to colestipol and loperamide, accompanied by abdominal bloating and cramping. Initial treatments with mesalamine and budesonide failed, and he discontinued budesonide due to hyperglycemia. On admission, he had stable vitals but exhibited electrolyte imbalances and acute kidney injury. Lab results showed hyponatremia (128 mmol/L), hypokalemia (2.9 mmol/L), hyperglycemia (224 mg/dL), and elevated creatinine (2.04 mg/dL). Hemoglobin was 10.3 g/dL, and WBC count was elevated at 14,100 cells/µL. He was started on IV fluids, potassium chloride, and methylprednisolone. After gastrointestinal consultation, his pancreatic enzyme dose was increased, and budesonide was restarted. Empiric antibiotics (ciprofloxacin and metronidazole) were initiated for possible infectious colitis. Sigmoidoscopy revealed diffuse moderately severe inflammation, ulceration, and friability, raising suspicion for ulcerative colitis. CT imaging showed colonic dilatation without significant wall thickening. Despite treatment, his diarrhea persisted, leading to the administration of infliximab, which resulted in symptom improvement. He also required total parenteral nutrition via a PICC line. The patient was discharged to rehabilitation in a stable condition.
Discussion: This case highlights the rare potential progression from collagenous colitis, typically considered benign, to ulcerative colitis (UC). There have been a few reports suggesting microscopic colitis (MC) can progress to IBD, though the mechanism remains unclear due to limited research articles and case reports available focusing on this topic. UC should be considered in MC patients presenting with acute symptom changes. Patients with this progression from MC to inflammatory bowel disease (IBD) are reported to be at risk for serious complications such as megacolon and perforation. The development of severe inflammation in this patient underscores the need to consider biologic therapies, especially in steroid-resistant cases. Elderly patients with complex histories, such as this patient’s malnutrition and chronic diarrhea, may present greater management challenges. In this case, refractory symptoms required escalation to biologic therapy, with infliximab providing symptom resolution. Comprehensive care, including nutritional support, was crucial in the patient’s management.
Conclusions: This case underscores the potential for microscopic colitis to progress to ulcerative colitis, particularly in elderly patients. Resistance to standard therapies in this case necessitated the use of infliximab, which ultimately led to clinical improvement. Clinicians should be aware of this potential progression and consider biologic therapies for refractory cases. Further research is needed to understand the pathophysiology of this transition and to guide optimal treatment strategies in complex cases like this one.