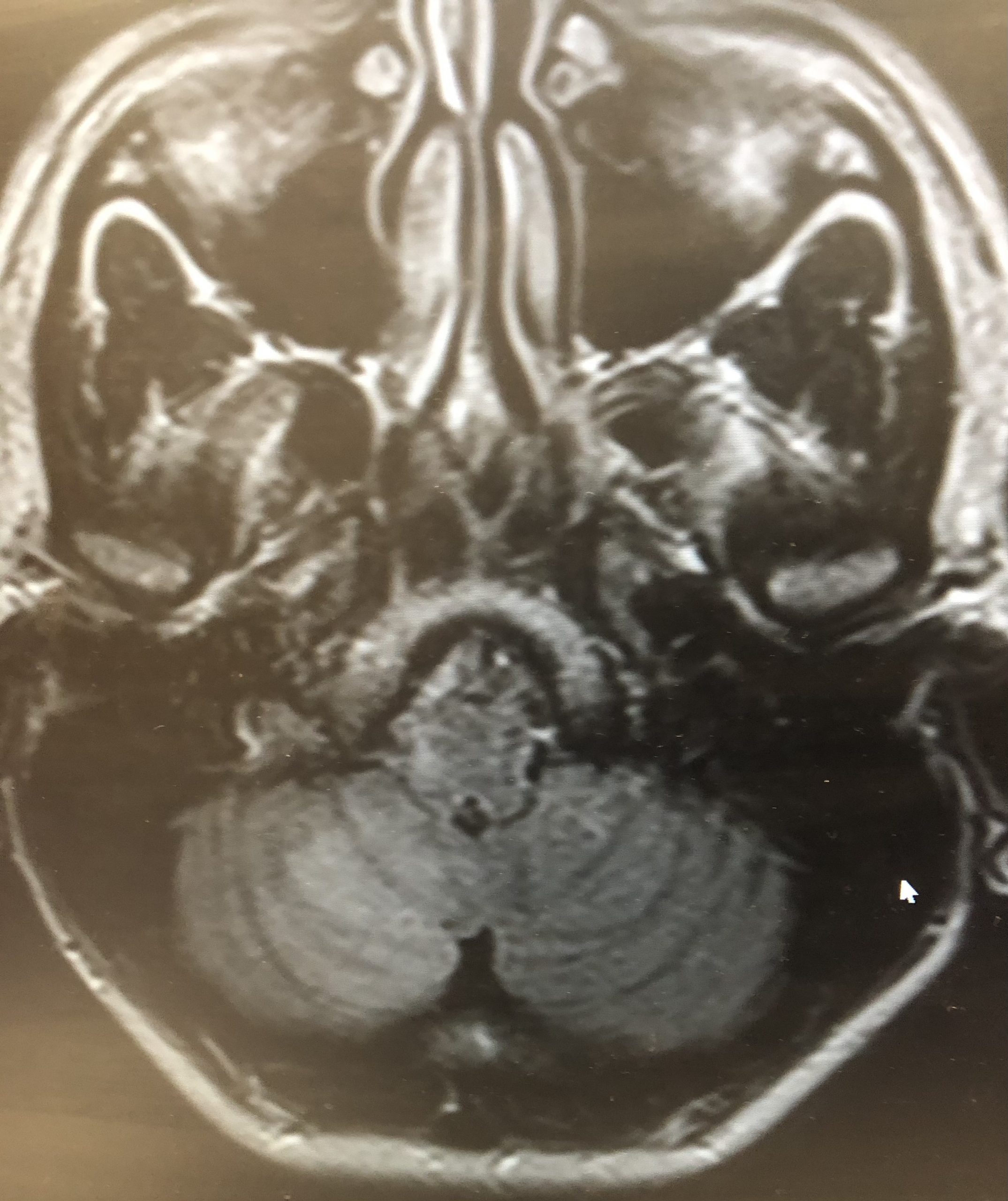
Case Presentation: A 33-year-old female with a history of limited Scleroderma diagnosed in 2015 and prescribed Methotrexate but non-adherent to same, presented to the Emergency Room with one day of acute onset dizziness associated with nausea and vomiting. An urgent CT head was performed, which was negative for acute intracranial pathologies. The patient was discharged home with a course of Meclizine. One day later, the patient re-presented with the same dizziness with new onset dysphagia coupled with right-sided facial numbness and left arm numbness. On examination, the patient’s vitals were unremarkable. Physical exam was significant for bilateral horizontal and rotatory nystagmus, increased P2 on cardiac auscultation and hyper-pigmented morphea lesions on bilateral anterior thighs and forearms. Lab work was significant for positive ANA with 1:320 speckled titer and positive anti U1 RNP antibody with negative anti-SS-A/SS-B, normal lipid panel, normal CRP and ESR with negative pro-thrombotic workup. MRI Brain revealed a 3 cm region of restricted diffusion in the right inferio-medial cerebellum extending to both the right cerebellar tonsil and right lateral medulla along with multiple acute infarctions in the right cerebellum. CT angiogram of the neck and brain revealed steno-occlusive disease with a laterally directed 3mm left posterior communication artery aneurysm. Additionally, there was a thromboembolic occlusion of the right vertebral artery V4 segment and a 4mm left ICA posterior lateral wall aneurysm which was presumed the likely source of the stroke. She then underwent a conventional angiogram which confirmed thromboembolic occlusion of the right vertebral artery without dissection.The patient was managed per acute ischemic stroke protocol with Aspirin 81mg and high dose statin. She received physical therapy, where she showed subsequent improvement in neurological defects. She was discharged after eight days with outpatient follow-up.
Discussion: There is a paucity of literature regarding presentation of ischemic neurovascular disease in scleroderma, an already poorly understood autoimmune disease. To the best of our knowledge, there have been few case reports published describing similar events of large thrombotic lesions in the cerebral vasculature. The pathogenesis is complex and has not been fully delineated, nonetheless, can possibly be explained by vascular dysfunction including elevated endothelin1 which promotes fibrosis, disequilibrium of nitric oxide and superoxide anions leading to vascular injury (1). In 16% of cases of SSc, neurological symptoms precede cutaneous manifestations (2). Of particular interest, in this case, is the patient’s cutaneous manifestation appeared first leading to her diagnosis. Additionally, of peculiarity is her short chronicity of illness leading to significant thrombosis of her posterior cerebral vasculature compounded with multiple acute on chronic infarcts mimicking embolic CVA . A study by Chiang et al. showed that SSc patients without previous stroke have a 43% higher risk of developing ischemic stroke in comparison to healthy control, also revealing that conventional treatment did not modify this risk (3).
Conclusions: Further research and development of standardized guidelines regarding screening, management and follow up for these patients may allow for alleviation of the significant disease burden involved in Scleroderma and may improve patient morbidity and mortality.