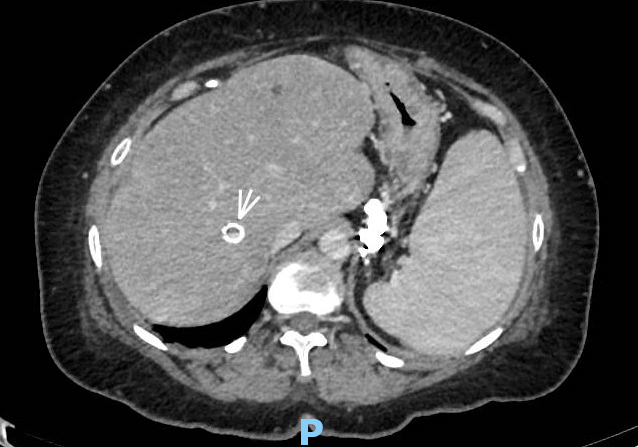
Case Presentation: A 63 year-old woman with a history of liver transplant presented to a rural hospital for evaluation of rigors, nausea and vomiting. Her post-transplant course had been complicated by HCV recurrence treated successfully with interferon and ribavirin; cirrhosis, and refractory gastric variceal bleeding for which she received a transjugular intrahepatic portosystemic shunt (TIPS) five years prior. Three months ago, she developed ESBL Escherichia coli (E coli) bacteremia treated with a ten-day course of ertapenem. She was readmitted a week later with recurrent E coli bacteremia due to endotipsitis requiring TIPS thrombectomy, and six weeks of ertapenem. Additionally, she underwent bare-metal stenting for occlusion of portal end of TIPS. On this most recent presentation, blood cultures (BC) from hospital day (HD) 1 revealed Enterobacter cloacae and meropenem was initiated. On HD 7, BC further revealed Candida glabrata and micafungin was started. She was transferred to our institution on HD 9. Upon arrival, vital signs revealed a heart rate (HR) of 114/minute, blood pressure (BP) of 142/79 mmHg and temperature of 38.2 º C. Cardiac examination was remarkable for normal S1 and S2 with no murmur; chest was clear to auscultation bilaterally and abdomen was non-tender. Laboratory data included a WBC count of 4,300 cells/mm3, hemoglobin of 9.2 gm/dL and platelet count of 70,000/mm3. Serum sodium was 134 mmol/L, creatinine 0.9 mg/dL, albumin 2.8 gm/dL, AST 33 U/L, ALT < 6 U/L, bilirubin 1 mg/dL and INR 1.3. Her MELD score was 9. BC revealed Candida glabrata and albicans, micafungin was continued. Abdominal CT revealed non-occlusive TIPS thrombosis and no ascitis. No infectious source could be identified from a transthoracic echocardiogram or chest radiograph. The patient underwent suction thrombectomy of mid-TIPS thrombus and thrombus biopsy yielded yeast forms and hyphae. Immediate post-thrombectomy course was complicated by recurrence of sepsis and candidemia, but continuation of micafungin led to BC clearance from HD 5.
Discussion: TIPS is commonly employed to treat patients with refractory ascites or recurrent variceal bleeding. 1,2 Endotipsitis, a rare complication of TIPS procedure was first described by Sanyal et al to describe sustained bacteremia associated with endovascular infection of TIPS stents. 3 Sustained bacteremia has been commonly defined as two blood cultures drawn > 12 hours apart that were positive for the same organism. 4 Endovascular infection is definitively diagnosed by culturing thrombotic material obtained from direct in-stent biopsy, 5 although demonstration of TIPS stenosis or thrombosis by imaging in the setting of bacteremia or fungemia may also suggest this diagnosis. Fever is the most common manifestation of endotipsitis, but other features such as chills, diarrhea, jaundice and shock have been described. In comparison to bacterial endotipsitis, fungal infection is rare, occurs later and is associated with > 60% mortality. 6 Prolonged antifungal therapy may be employed, similar to recommendations for bacterial endotipsitis. Even though TIPS removal would be optimal, the role of liver transplantation remains unclear in these patients, as is the need for chronic antifungal therapy. 7
Conclusions: Fungal endotipsitis should be considered in any post-TIPS patient with recurrent bacteremia or fungemia despite adequate antimicrobial therapy. More studies are needed to evaluate the role of transplantation and aggressive medical therapies.