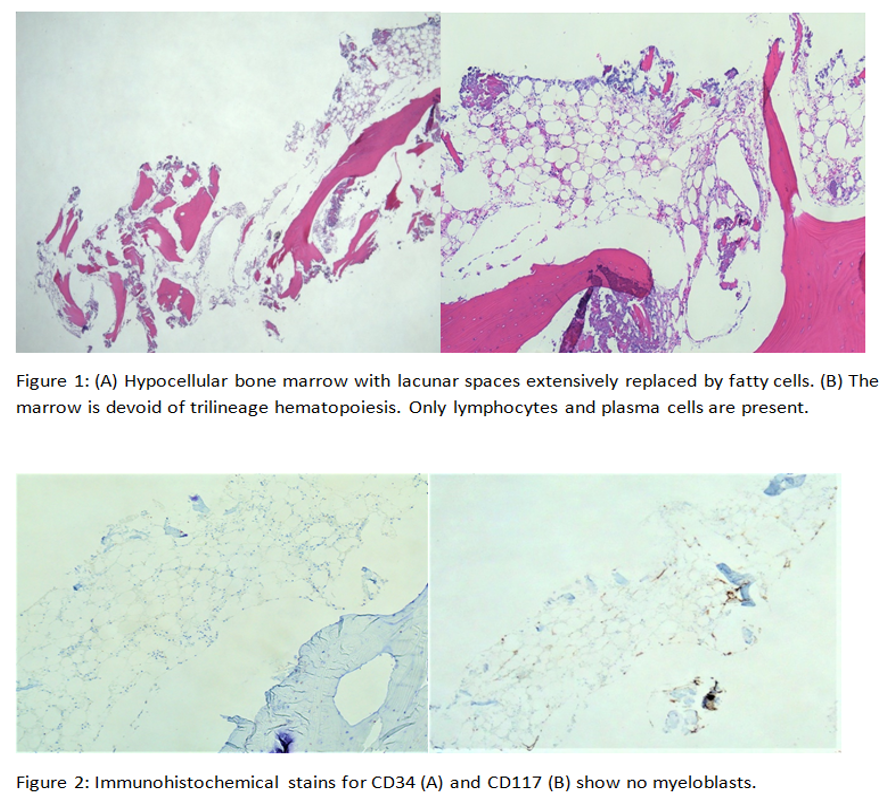
Case Presentation: Our patient is a 42-year-old Hispanic female with a past medical history of hypothyroidism, iron deficiency anemia, and onychomycosis. She presented with complaint of generalized bruising all over her body for last 2 days. The patient reported that she was in her usual state of health except that she was started on Terbinafine for recurrent fungal nail infection two months ago. Her complete blood count at that time revealed WBC 6.2 , platelet 380 K/CMM, Hgb 9.4 g/dl, MCV 74 fl, Ferritin 3 ng/ml, TSH 4.80. Patient mentioned that she initially started noticing bruising over her right gluteus, left calf, abdomen, and right forearm 2 days prior to admission. The patient denied any trauma or recent fall. The patient reported that she had a similar bruise over anterior chest last year and was taking terbinafine at that time. On admission, physical examination revealed scattered petechiae over anterior chest and ecchymosis on left calf (3×4 cm), right gluteus (2×2 cm), and right lower abdomen (1×2 cm). No lymphadenopathy or organomegaly were noted. Her labs revealed pancytopenia: Hgb 9.2 g/dl, platelet count 6 k/CMM, WBC 2.1 K/CMM, ANC 0.4 K/CUMM. A peripheral blood smear was consistent with pancytopenia, no schistocytes or spherocytes noted. The reticulocyte count was low 0.009, LDH, fibrinogen, D-dimer, LFTs, KFTs, TFTs, vitamin B12, and folate levels were within the normal limit. A CT chest, abdomen, and pelvis and a USG doppler of lower extremities were unremarkable. The patient tested negative for HIV, Viral Hepatitis, EBV, and Parvovirus. A flow cytometry revealed no immunophenotypic evidence of B cell or T cell non-Hodgkin lymphoma or acute leukemia. Bone marrow biopsy reported only Lymphocytes and plasma cells consistent with Aplastic anemia.Her pancytopenia was attributed to terbinafine, and it was held. Her hospital course was complicated by a neutropenic fever on day 6 for which she was treated with cefepime. Blood culture and urine culture remained negative throughout her course. The patient started her menstrual cycle on day 7 and her Hgb dropped to 6.6, which improved to 8.2 after a 2U PRBC transfusion.She was transferred to the ICU for closer monitoring for severe thrombocytopenia and a platelet count 2 K/CMM. The patient received 16 Units of platelets and 6U PRBC during her hospital stay. Due to persistent pancytopenia and profound neutropenia with ANC 0 K/CUMM, decision to administer immunosuppressive triple therapy (hATG+cSA+Eltrombopag) was made. Her counts started to improve after 2 weeks with the therapy and she was discharged home with an outpatient follow-up with hematology.
Discussion: Onychomycosis (OM) is a common skin fungal infection of the nails that is caused by dermatophytes, nondermatophytic molds, or yeast. It has a high prevalence and is associated with significant morbidity. Systemic antifungal agents are the gold standard for treatment. While terbinafine inhibits fungal squalene epoxidase, it can also inhibit mammalian enzymes and therefore decrease blood cell production in bone marrow. Here we report a case of aplastic anemia associated with oral terbinafine use that improved with the use of immunosuppressive therapy.
Conclusions: Terbinafine, although considered safe and well tolerated, can have the rare yet serious side effects of bone marrow suppression and aplastic anemia. Patients should be educated and serial labs can be helpful for those who are on a chronic course of terbinafine. Early diagnosis and the start of treatment can lead to a favorable outcome.