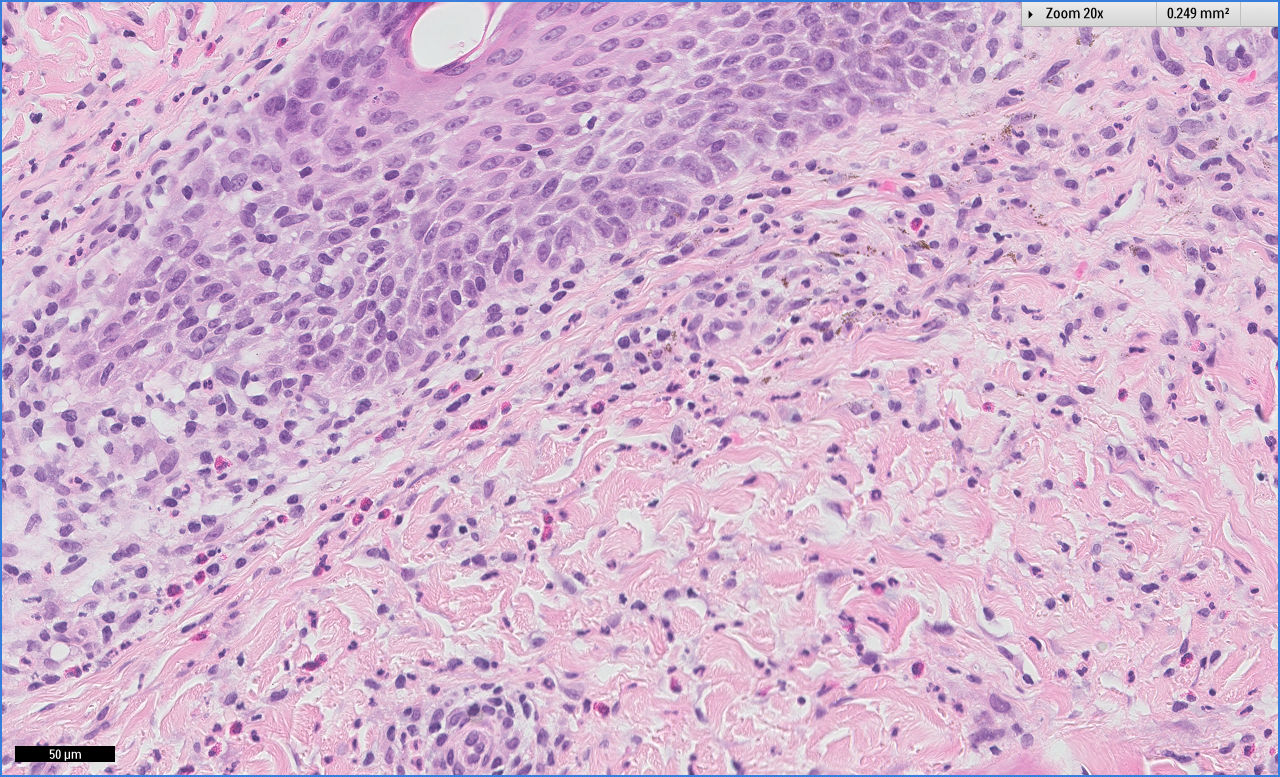
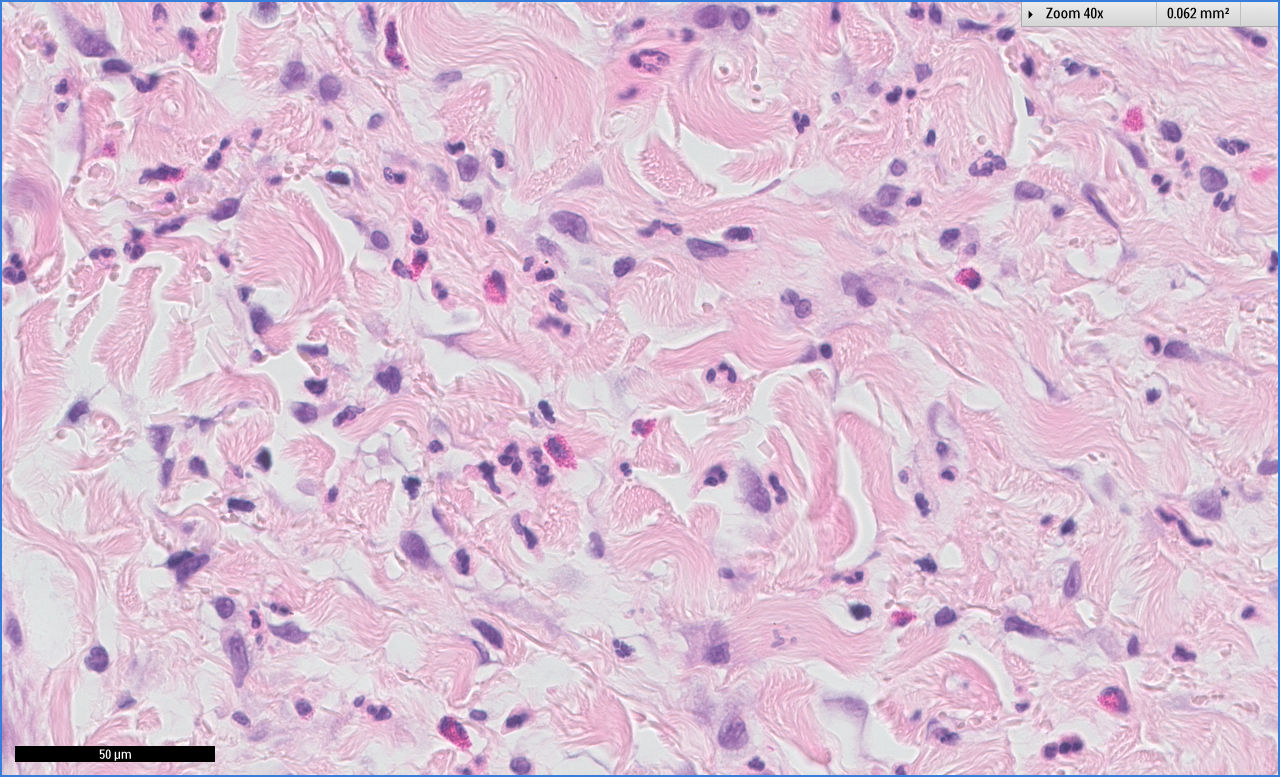
Case Presentation: The patient is a 29-year-old female with the history of acute pancreatitis and gastric bypass surgery, who initially presented with lower extremity swelling in the setting of hypoalbuminemia and protein-calorie malnutrition. She was started on high calorie/protein diet and was discharged on furosemide. Three weeks after discharge, she noticed peri-oral rash, which extended to lower extremities, groin, and trunk. On presentation, she had multiple areas of erythema and crusting over the body with small tense vesicles of legs and bilateral lower extremities edema. Blood work showed elevated liver enzymes, elevated INR, low vitamin D, normal hemoglobin and elevated eosinophils. She underwent left forearm skin biopsy, which showed findings consistent with drug hypersensitivity. She was diagnosed with DRESS syndrome and was started on Prednisone secondary to liver dysfunction. Her liver function improved and rash resolved. She was discharged on Prednisone for outpatient slow taper. She presented again with complaints of weakness, fatigue, and dyspnea on exertion. Completed blood count showed hemoglobin 8.5 gram/dl, which later dropped to 7.1 gram/dl. No source of bleeding was identified. Hemolysis work-up came back positive with elevated LDH, low haptoglobin, elevated reticulocyte count and positive Coombs test. She received IVIG therapy and continued with Prednisone. Her hemoglobin levels remained stable without any further drops. She completed outpatient Prednisone taper over 6 weeks and her hemoglobin normalized to 12.1g/dl on 6 months follow up, without any recurrence of hemolysis.
Discussion: DRESS syndrome is a severe delayed-type hypersensitivity (type IV hypersensitivity) reaction with a prolonged latency period of 3-8 weeks and symptoms may persist for a longer period of time, despite discontinuing the offending drug. Although fever and rash are the most common presentations, the defining characteristic is organ dysfunction. The pathogenesis involves activation of helper T cells in the skin secondary to interaction of medications. RegiSCAR is the most commonly used point-based scoring system to diagnose DRESS syndrome. In some patients with DRESS, long-term complications such as end-organ damage and autoimmune disorders, specifically autoimmune hemolytic anemia, Graves’ disease and type 1 diabetes mellitus have been observed. Systemic corticosteroids are the treatment of choice especially in patients with liver dysfunction. IVIG is reserved for patients with life-threatening conditions such as respiratory failure, hemolytic anemia or renal failure.
Conclusions: Drug reaction with eosinophilia and systemic symptoms (DRESS) is a life-threatening adverse drug reaction with mortality rates of up to 10-20%. Although aromatic antiepileptic agents are the common culprits, Sulfonamides are also associated with DRESS syndrome in rare cases. We report a rare case of DRESS syndrome complicated by liver dysfunction and autoimmune hemolytic anemia (AIHA) secondary to furosemide. DRESS syndrome should be kept in differentials in patients with rash and organ dysfunction after taking Furosemide.