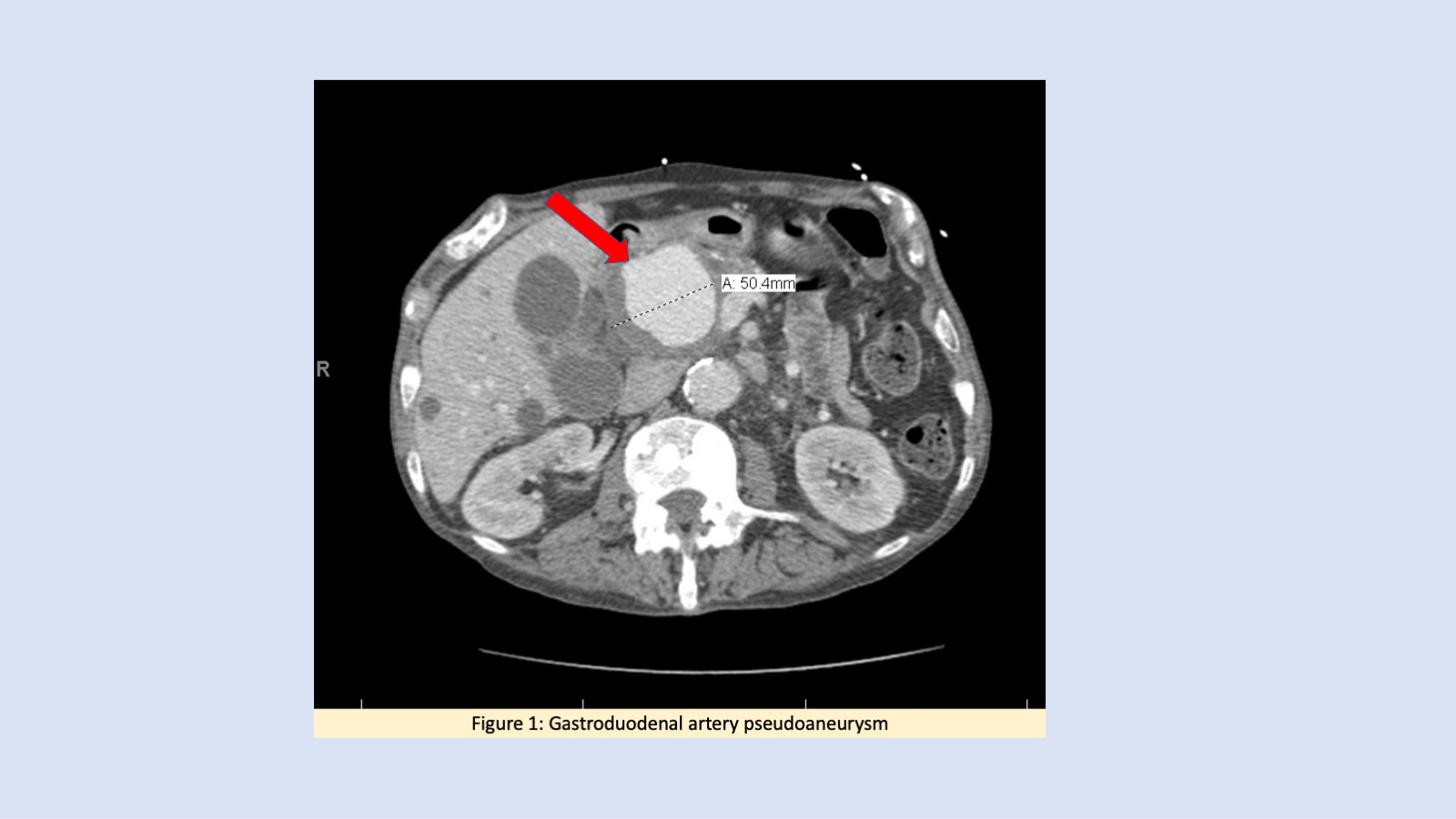
Case Presentation: A 69-year-old male with history of metastatic prostate cancer on chemotherapy presented with fever for three days. On presentation, he was tachycardic with a heart rate of 130 beats per minute. Physical examination was significant for right upper quadrant tenderness. Initial laboratory workup revealed leukocytosis with a white blood cell count of 17000 cells per cubic millimeter and elevated alkaline phosphatase with hyperbilirubinemia. Infectious workup including chest X-ray, blood, and urine cultures were unremarkable. He was empirically started on cefepime for treatment of sepsis of unclear etiology. Abdominal Computed tomography scan revealed a 5.3 x 5.4 cm GDA aneurysm [Figure.1] with associated common bile duct compression leading to hepatic ductal system dilatation. Vascular surgery recommended immediate intervention and patient underwent endovascular stent placement of the GDA arising from hepatic artery and coil embolization of feeder branches from superior mesenteric artery. Further infectious workup to identify the source of infection including a transthoracic echo were unremarkable. Given the high suspicion of a mycotic aneurysm, patient was discharged on intravenous ceftriaxone to complete a four-week course.
Discussion: Visceral artery aneurysms are unusual entities associated with high mortality in cases of rupture. Gastroduodenal artery (GDA) aneurysms are rare and comprise 1.5% of all visceral aneurysms [1]. GDA aneurysms can be either true or pseudoaneurysms. In the latter case, it can be secondary to an intraabdominal inflammation, post-procedural, or rarely mycotic [2]. It is rare for GDA aneurysms to present as CBD obstruction causing cholestatic transaminitis and hyperbilirubinemia. Visceral aneurysms usually can arise after acute or chronic pancreatitis, recent instrumentation, or due to an infectious source. Endovascular intervention should not be delayed due to high risk of rupture and intrabdominal bleed [3]. Abdominal imaging should be performed when obstructive jaundice is suspected to rule out these rare entities as delay may be associated with a higher risk of complications.
Conclusions: Evaluation of cholestatic transaminitis should include abdominal imaging to identify rare etiologies such as visceral aneurysms prompting timely intervention