Background: Geographic localization (GL) has been shown to improve perceptions of physician-nurse, physician-physician, and physician-Case Management communication. However, data on other benefits of GL are mixed. While some studies show that GL improves time allocated by physicians for direct patient care, others report an increased frequency of workday interruptions and greater time spent on indirect care. Similarly, GL initiatives have been associated with mixed impacts on patient length of stay (LOS). We report the impact of a GL initiative (Plan-Do-Study-Act or PDSA cycle 1) on LOS at a 700-bed, level 1 academic medical center.
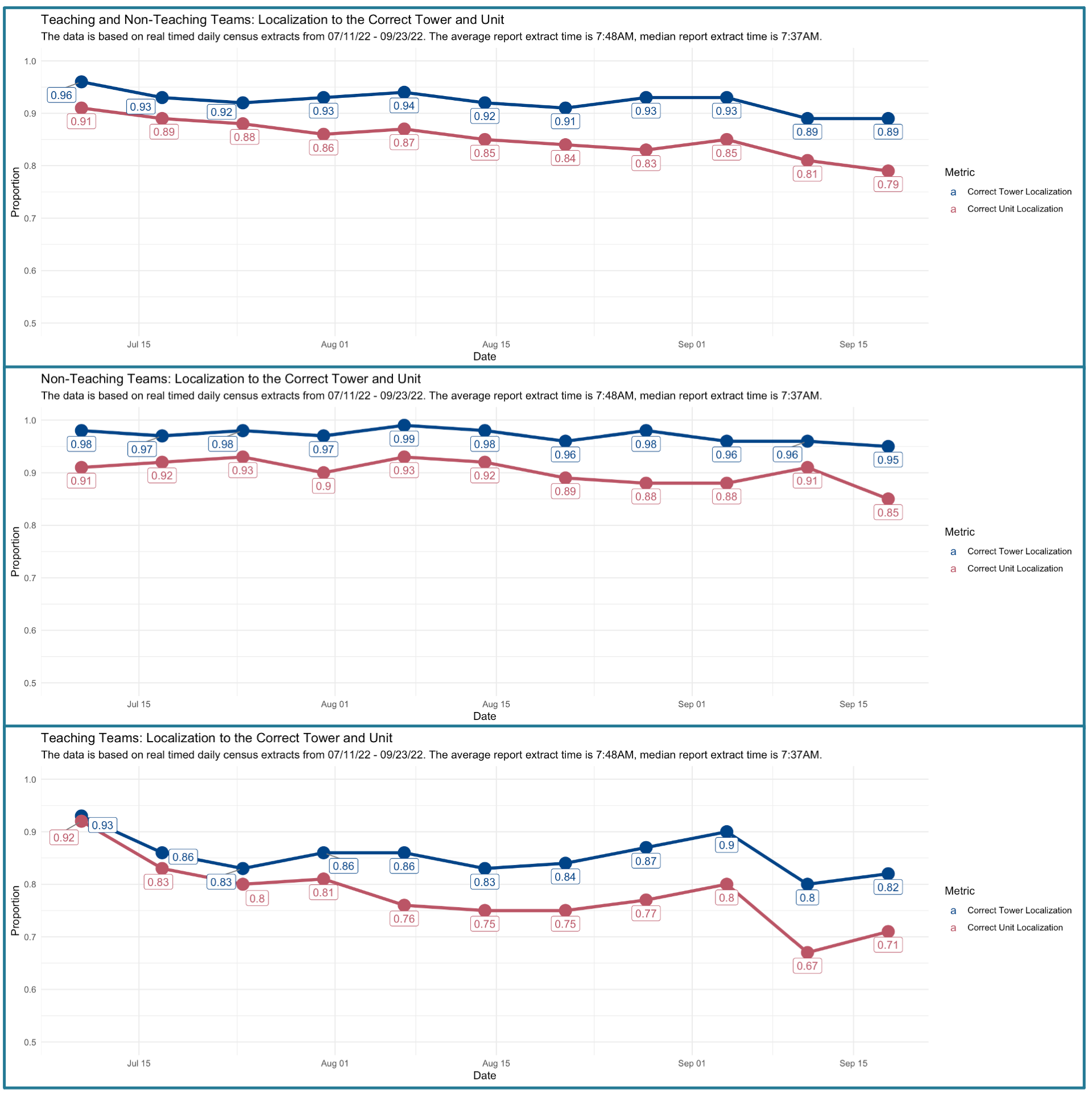
Methods: Inpatient beds at our hospital are located on two “towers,” each housing several inpatient units. There are five designated medicine units. Before 07/11/22, we attempted GL by assigning each of the 16 inpatient hospital medicine (HM) teams to 1 or 2 units. We have traditional house staff teams and nine direct care teams. Admissions to HM teams are accepted through a physician triage hospitalist (triagist). Prior to 07/11/22, bed planning would attempt to assign patients to designated floors based on the team assigned by the triagist, i.e., a team-before-bed model. We assembled a multidisciplinary group of hospitalists, case managers, bed planning personnel, and nurses to design a new localization model. Several interventions were implemented. First, we started admitting patients to a “transitional team” with the goal of rounding team assignment after patients had been assigned an inpatient bed, i.e., a bed-before-team model. Second, patients boarding in the emergency department at 7 am were pre-assigned to units based on anticipated discharges by bed planning. Third, twice-a-day multidisciplinary discharge planning rounds were initiated on each localized floor. Finally, a patient reshuffle was performed each week to coincide with hospitalist switch day, where patients who had been misassigned to a non-localized team were reassigned to the team localized to the correct floor. Our goal was to achieve a 90% same-tower GL and an 80% same-unit GL while improving our LOS. Secondary outcome metrics monitored included Risk-Adjusted (RA) 30-day readmissions and RA-Mortality.
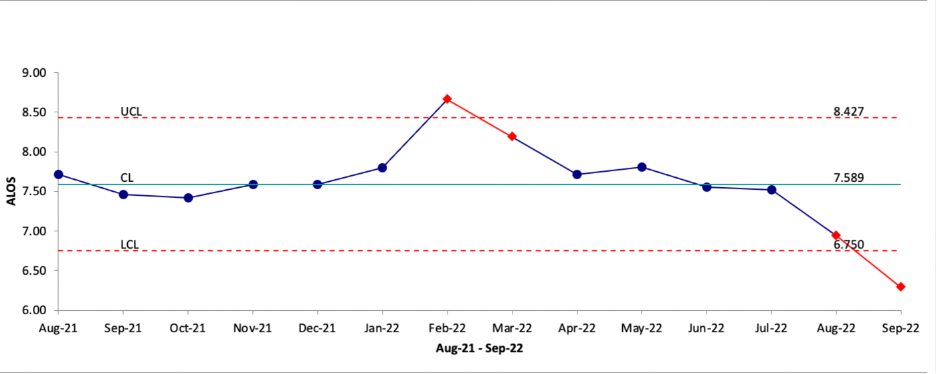
Results: We present our results two months after implementing the new localization model. House staff teams had an average correct tower (CT) and correct unit (CU) GL rate of 85.45% and 77.91%, respectively. Direct care teams had average CT and CU GL rates of 97.09% and 90.18%, respectively. All teams, in aggregate, had an average CT and CU GL rate of 92.27% and 85.27%, respectively. After implementing GL, we saw a decline in the Average Length of Stay (ALOS) in August and September (figure 1). This decline in LOS constitutes a non-random, special cause variation. Mortality increased from 0.498 to 0.586 (p > 0.05), and RA-30-day readmissions decreased from 0.791 to 0.712 (p > 0.05).
Conclusions: Our process improvement project provides a template to attain GL in busy hospitals that consistently operate at greater than 100% capacity. We also see a decrease in ALOS early on in the first PDSA cycle of this project. This is likely due to robust multidisciplinary discharge planning with unit-based case managers and nursing staff that we were able to put in place for our localized teams. The second PDSA of this project will target a process metric of close to 100% CU GL with the goal of further improving LOS.