Background: More than two million people are evaluated for syncope each year in the United States, and approximately 30-40% of these patients are hospitalized for further costly investigation. Total annual cost of syncope related hospital evaluation is estimated to be over 2 billion dollars. The most common cause of syncope is reflex mediated. It does not increase mortality in patients under the age of 65.In geriatric patients syncope is associated with increased mortality irrespective of cause.Syncope is usually an isolated occurrence in younger patients whereas it is multi-factorial in elderly. We evaluated demographic characteristics, co-morbid condition, clinical presentation, ED evaluation data and composite adverse outcome (cardiovascular events, pulmonary embolism, bleeding, and death) at 48 hours and 30days and calculated two widely used syncope scoring system: Evaluation of Guidelines in Syncope Study (EGSYS) and San Francisco Syncope Rule (SFSR).
Methods: In this single center retrospective cohort study, we evaluated patients of age 65 or above presented to a large academic center with syncope during the period of 01/01/2017 to 12/31/2018. Patients with confirmed non-syncopal syndromes,acute medical condition, drug or alcohol use prior to the event were excluded from the study. Data on demographics, clinical presentation, laboratory, echo cardiogram, treatment and outcome were collected by retrospective chart review in redCap data management system. Data quality was assessed to minimize inter-observer variability using a representative sample from the cohort. At the completion of data collection EGSYS and SFSR scores were calculated and classified into low and high risk patients based on set criteria of the scoring system. Means and prevalence were calculated for different variables in overall study population. SAS version 9.4 was used for statistical analysis.
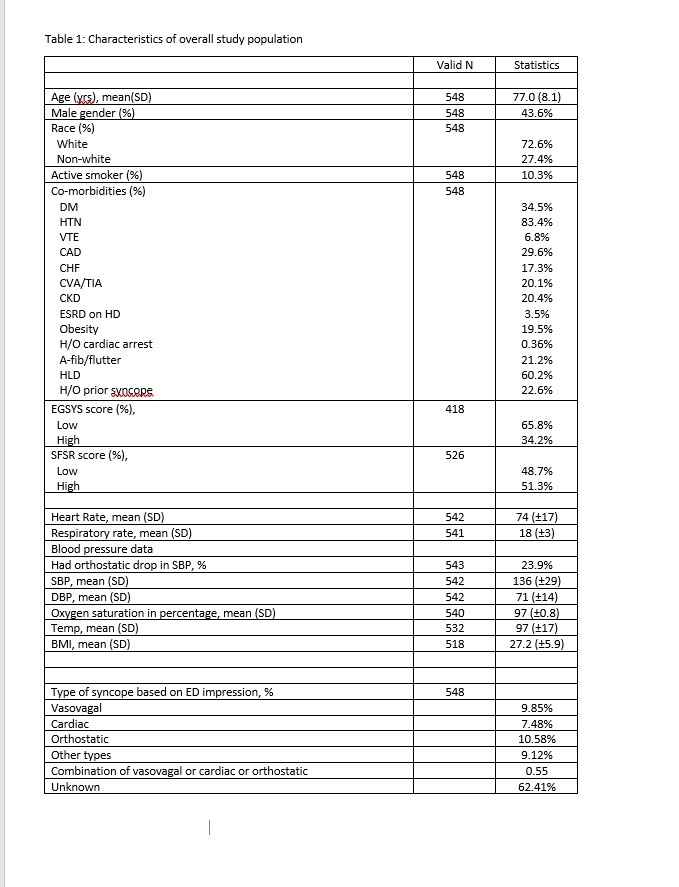
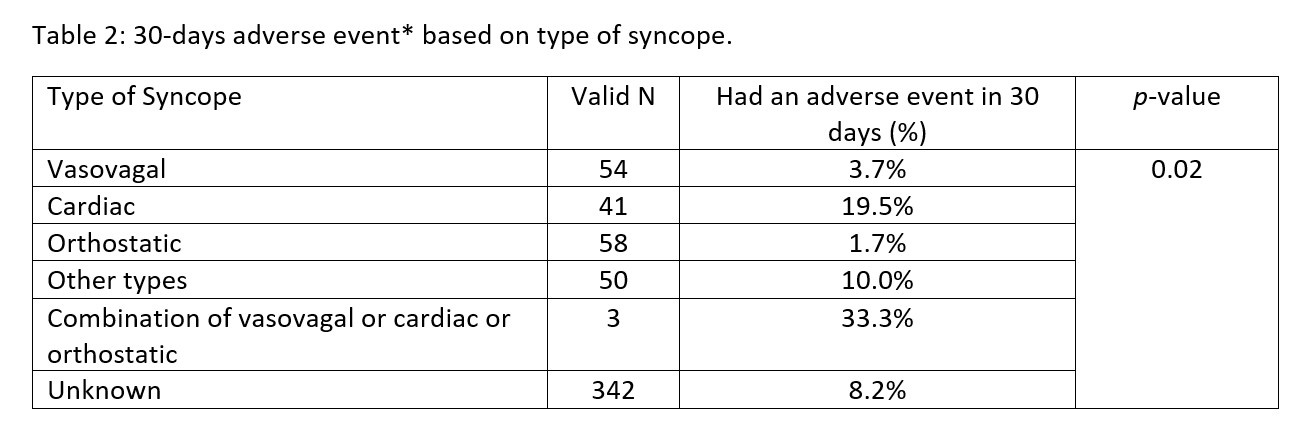
Results: After all exclusion criteria total 548 eligible patients’ charts were reviewed. Mean age was 77 (±8) years, 43.6% were male, 72.6% were white, mean BMI was 27.2(±5.9) and 10.3% were active smokers. Among co-morbidities, prevalence of hypertension and hyperlipidemia were highest (83.4% and 60.2%, respectively). Concomitant medication use were: calcium channel blocker 29.9%, nitrate 10.8%, beta blocker 45.8%, ACEI/ARB 47.3%, diuretics 42.1%, anti-depressant 36.6%, opiates 22.1%. Percentage of vasovagal syncope was 9.9%, cardiac syncope was 7.5%, orthostatic syncope was 10.6%, combination of three types were 0.55%, other types and unknown were 71.5%. 2.4% patients had composite adverse event at 48 hours and 8.2% at 30 days. Mean EGSYS and SFSR scores were 1.61 and 0.72 respectively, prevalence of high risk EGSYS and SFSR scores were 34.2% and 51.3% respectively.
Conclusions: Geriatric patient with sign-symptoms of syncope were mainly male gender and white race predominant. They had higher prevalence of hypertension and hyperlipidemia with majority of them using anti-hypertensive along with anti-depressant medications. Interestingly majority had undifferentiated type of syncope. These population had low prevalence of 48 hours adverse event rate compared to 30-days adverse events but high prevalence of high-risk scores. This finding is challenging our current practice of 24-48 hours observation practice in this age group. Further association analysis of different risk factors and performance of different scoring system in predicting adverse outcome is warranted.