Background: Lack of mobilization of hospitalized non-ICU medical patients has known negative consequences, including worse health and psychological outcomes, functional decline and increased hospital length of stay (1). Known challenges to increasing mobilization amongst inpatients include patient- and institutional-related limitations such as patient symptoms and lack of available assistance (2). At our urban, quaternary care, 1,100 bed academic medical center, we perceived that staff may experience additional obstacles that prevent consistent mobilization of inpatients, which can result in low value use of limited skilled physical therapy (PT) resources. In this study, our interdisciplinary team sought to assess physician knowledge and beliefs surrounding patient mobility on the Hospital Medicine service in order to identify center-specific contributors to low-value use of skilled PT and to target planned future interventions.
Methods: A 26-question validated survey (3) originally developed at Johns Hopkins was distributed to 36 Hospital Medicine attendings and 163 internal medicine interns and residents. Data was collected and analyzed by our team of a physical therapist, internal medicine residents and hospitalists.
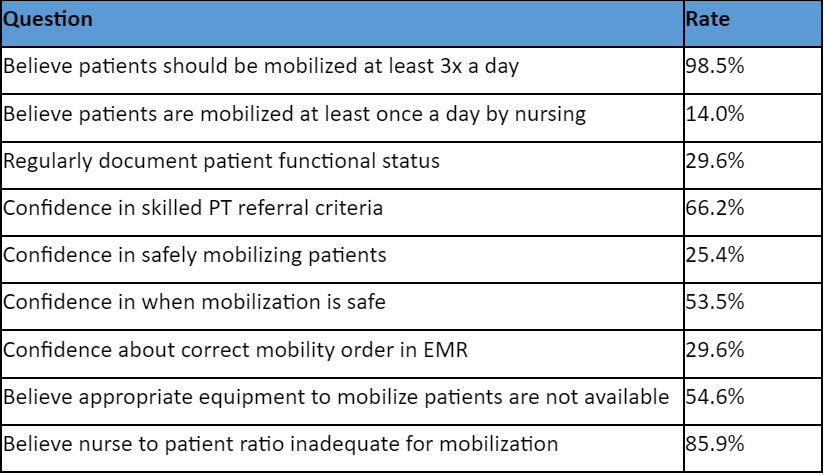
Results: A total of 71 of 199 (36%) providers responded to the survey (22 hospitalists (61%) and 49 internal medicine house staff (30%)). 98.5% of respondents believe that mobilizing appropriate patients at least three times daily will lead to better patient outcomes, but a minority (14%) believe their patients are mobilized at least once daily by nursing. 70.4% of respondents report not regularly documenting their patients’ physical functioning status, and 66.2% report confidence in skilled PT referral criteria, despite the fact that our center has a high percentage of inappropriate PT consults. Further, 74.6% of respondents feel unconfident in their ability to safely mobilize patients, half (46.5%) are unsure of when patient mobilization is safe, and over two thirds (70.4%) are unsure if patients have appropriate mobility orders in the electronic medical record (EMR). Finally, almost half (45.4%) of respondents believe that the proper equipment to mobilize patients is not readily available, and 85.9% believe that nurse-to-patient staffing ratios are inadequate to allow consistent patient mobilization.
Conclusions: These results demonstrate that while physicians almost unanimously agree that increased patient mobility will improve health outcomes, very few believe their patients are mobilized frequently enough. Perceived local barriers to patient mobility include a lack of documentation of patients’ baseline functional ability to allow targeted use of skilled PT, absence of formal physician education on patient mobilization and its contraindications, inaccurate EMR mobility orders, lack of accessible equipment, and inadequate staffing to mobilize patients. Our team will target these domains to improve high value use of skilled PT and increase patient mobility in our inpatient population.