Background: Hospitalization at Home (HaH) has demonstrated clinical quality and patient experience superiority in general inpatient medical patients. Expansion of this service to sub-specialized inpatient populations would be highly beneficial to patients and health systems. Mount Sinai Health System (MSHS) HaH enrolls oncology patients with active disease admitted for acute general medical conditions and for active chemotherapy. We describe our institution’s experience of HaH in oncology patients.
Methods: We performed a retrospective chart review of oncology patients enrolled in HaH from August 2019 to November 2022. Patient eligibility for HaH required meeting established institutional HaH admission criteria. We focused initial enrollment on patients with multiple myeloma admitted for elective chemotherapy and then managed on HaH through post chemotherapy management on a disease-specific clinical pathway. Demographics, cancer diagnosis, social situation, indication for antecedent ED or inpatient stay, and HaH admission were extracted from the electronic medical record. Our primary endpoint was rate of successful HaH admission, defined as discharge from HaH for complete recovery from the acute condition or transition to hospice. We also evaluated patient social support and home resources.
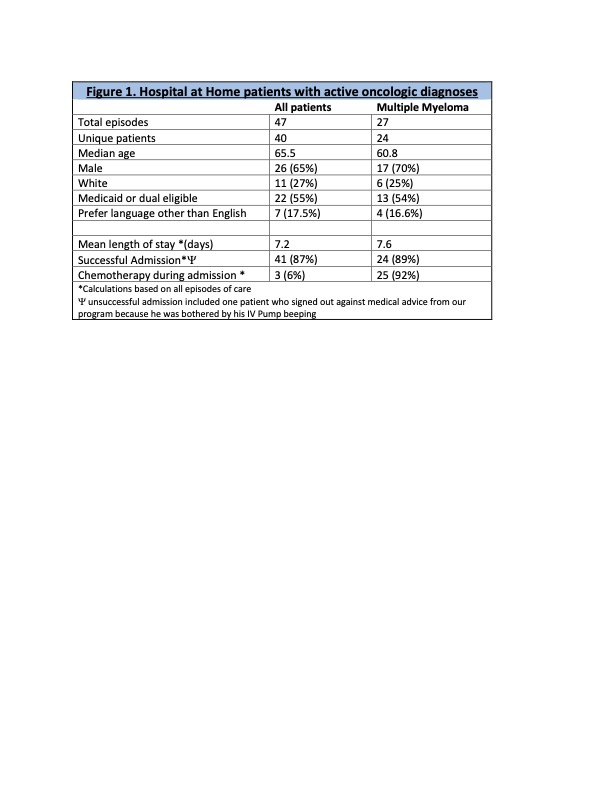
Results: We had 47 episodes of care, 40 of whom were unique patients with the following cancer types: multiple myeloma (n=24), solid oncology (n=14), and one each lymphoma and leukemia. Overall, the median age was 65 years, 65% (n=26) were male, 27% (n=11) were white, more than half (55%) had either Medicaid or were dual Medicare/Medicaid eligible, and 17% (n=7) preferred another language other than English. For the multiple myeloma patients, the median age was younger at 60.8 years. All but 2 patients in the multiple myeloma cohort were admitted for continuing treatment post-chemotherapy. Successful admissions occurred for 87% (n=41) of all patients and 89% (n=24) for the multiple myeloma cohort. Mean length of stay was 7.2 days for all patients, which saved our health system 340 inpatient-bed days. No significant adverse outcomes or issues related to the care delivery or social support.
Conclusions: The MSHS HaH program demonstrated safety and feasibility in caring for patients with active oncologic diagnoses and for patients admitted for elective chemotherapy. We were able to successfully care for the majority of cancer patients with a significant savings in inpatient bed days. HaH should be expanded to other groups of specialized patients, leveraging disease-specific clinical pathways.