Background: Throughput is a challenge for many hospitals. Discharging patients impacts throughput, but is time-consuming and competes with other physician and nurse tasks, often being left on the “back burner” while attending to sicker patients. Discharge paperwork, patient education, and ride coordination are often incomplete when patients are ready for discharge, adding to delays. Prior models of care have shown improved outcomes with individualized discharge plans and unit based case managers, while discharge times have remained harder to improve.
Purpose: Our primary objective was to improve the quality and timeliness of discharge by identifying patient needs from the start of the hospital stay and completing the majority of work related to discharge early in the hospitalization
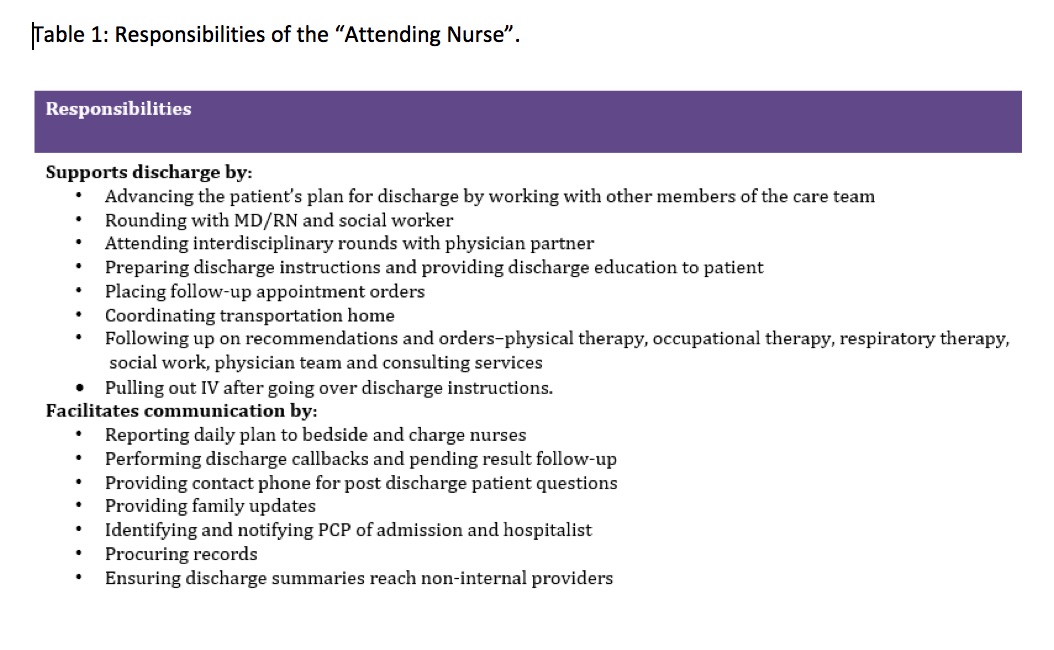
Description: A multidisciplinary workgroup including physicians, nurses, and social workers created a process map of all tasks related to a hospital discharge. While discussing barriers to discharge, the new role of Attending Nurse (AN) was established. The AN is an experienced nurse whose primary focus is preparing for and executing discharges. Different from a case manager, the AN is paired with a hospitalist physician and shares the same panel of patients. The hospitalist and AN round on patients together and attend interdisciplinary rounds. The AN proactively identifies patient discharge needs from day one of hospitalization. They also prepare discharge paperwork, provide patient education, and communicate anticipated discharge dates and post-discharge plans to patients and families.
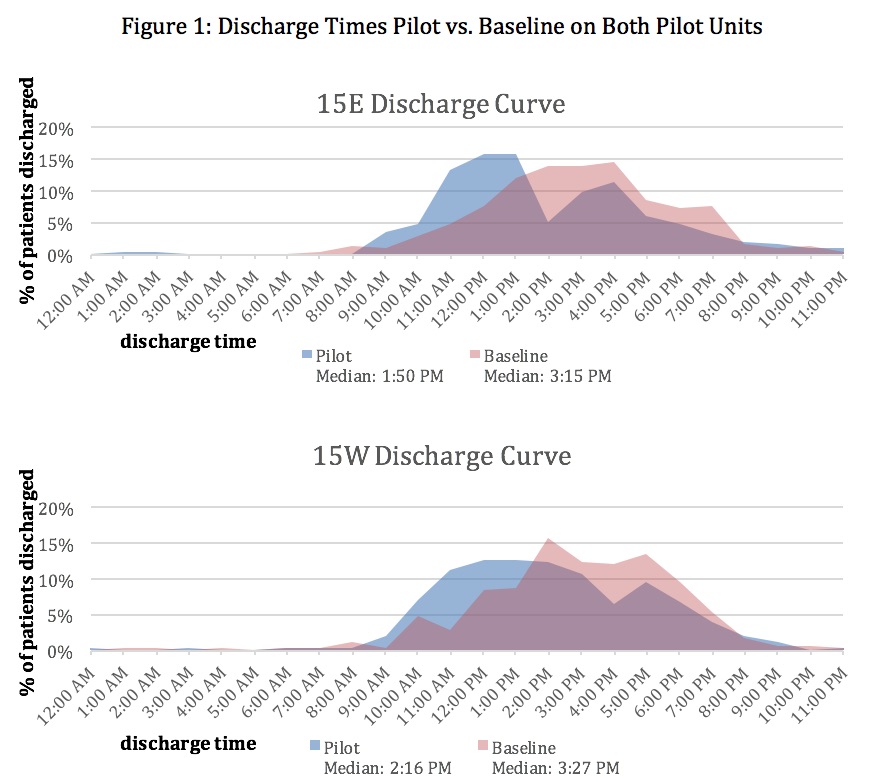
We piloted the AN role on two of four general medicine hospitalist units. On the pilot units, the median discharge time was seventy- one and eighty-five minutes earlier than baseline with median discharge times of 1:50pm and 2:16pm. Median admission times of patients to the pilot units also improved by seventy and seventy- two minutes. Response from staff nurses, social workers, and hospitalists was positive. The AN role was highlighted as the most positive change during the past year on the annual division of hospital medicine work-life survey. HCAHPS comments demonstrated a positive impact on patients, as noted by patients writing favorable responses describing efficiency of the discharge process.
Conclusions: The Attending Nurse partners with hospitalists and focuses on making the discharge process efficient. Establishing this role can impact throughput by shifting discharge and admission times to earlier in the day.