Background:
Vitamin D deficiency is common in elderly patients with low‐trauma hip fractures, and major practice guidelines recommend screening for deficiency in this population. Our hospitalist group admits all patients with acute hip fracture, with co‐management by orthopedics. Our group had no standardized approach to assessment of and treatment for vitamin D deficiency in this population.
Purpose:
To standardize and improve group practice for the assessment of and treatment for vitamin D deficiency in elderly patients with hip fracture.
Description:
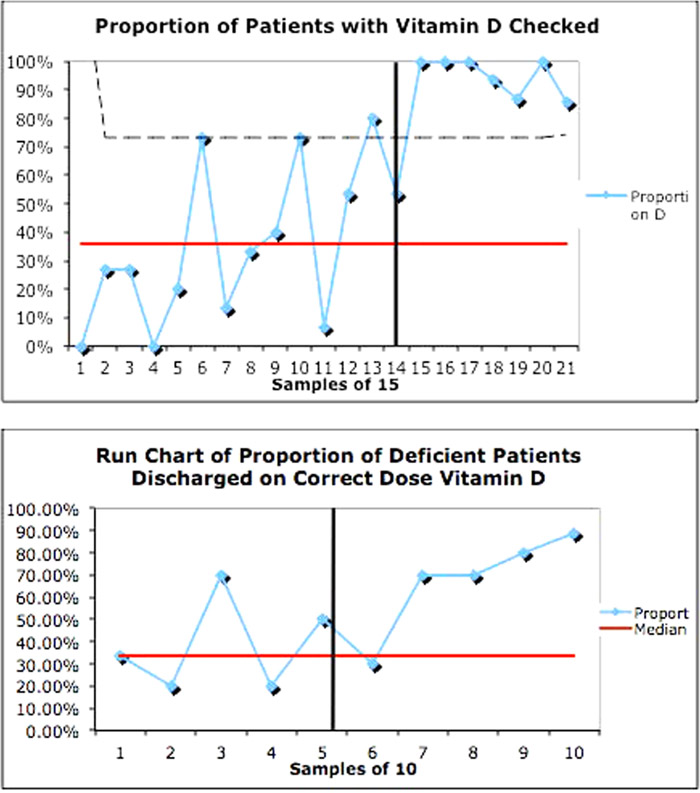
We reviewed medical evidence, including major practice guidelines, for screening for vitamin D deficiency in elderly patients with low‐trauma hip fracture and assessed our group’s adherence to best medical evidence. Review of all hip fracture patients cared for by our group from June 2010 through October 2012 revealed only 38% had been assessed for vitamin D deficiency. Of those patients who had a level checked, 61% were found to be vitamin D deficient using a cutoff of <30 ng/mL. Of those deficient, only 39% were treated with the appropriate dose of vitamin D. Our conclusion was that group performance on this issue was varied and substandard.
In October 2012, we created an intervention to address these findings. We presented a review of evidence and data from our practice to the hospitalist group. Concurrently, we altered the hip fracture order set in the hospital computerized physician order entry system to include prechecked boxes for measurement of vitamin D level at admission and empiric supplementation with 1000 international units of vitamin D.
We studied implementation of the new order set by searching the hospital database for ICD‐9 codes for femoral neck fracture linked with discharge physicians in our group. Outcome measures included the percentage of patients screened for vitamin D deficiency and percentage of deficient patients discharged on the correct dose of vitamin D, both before and after intervention. We also describe the prevalence of vitamin D deficiency in this population.
Following our intervention, 95% of hip fracture patients were checked for vitamin D deficiency, compared with 38% before intervention. More patients with vitamin D deficiency were discharged on the correct dose of supplemental vitamin D, going from 39% to 67%. Prevalence of vitamin D deficiency was 49.5%.
Conclusions:
Prevalence of vitamin D deficiency in elderly hip fracture patients is high. Our hospitalist group practice performance in screening for vitamin D deficiency in this population was varied and not in adherence with current practice guidelines. With a review of best evidence and alteration of the hip fracture computerized physician order entry order set, we successfully standardized group practice and improved adherence to practice guidelines.