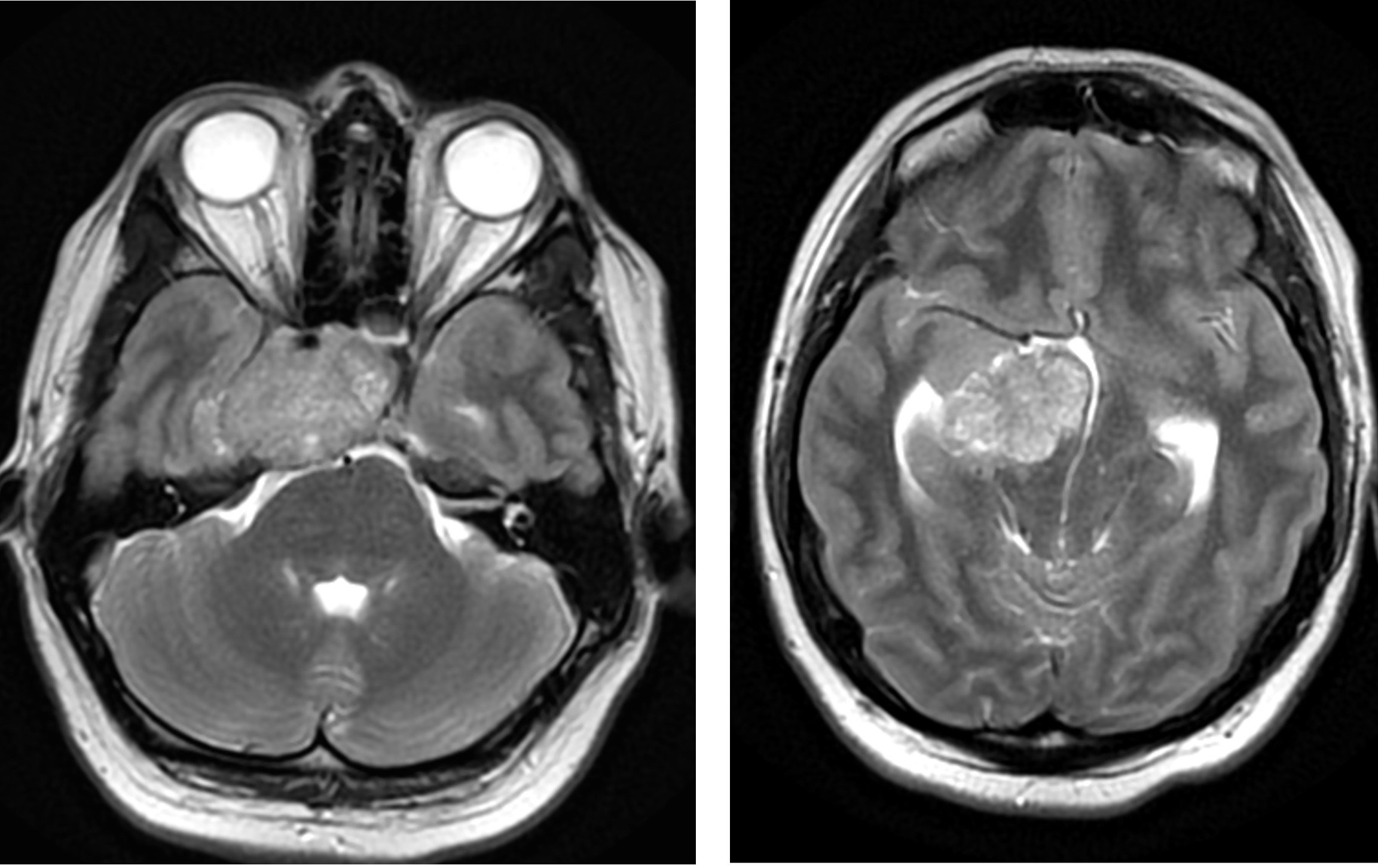
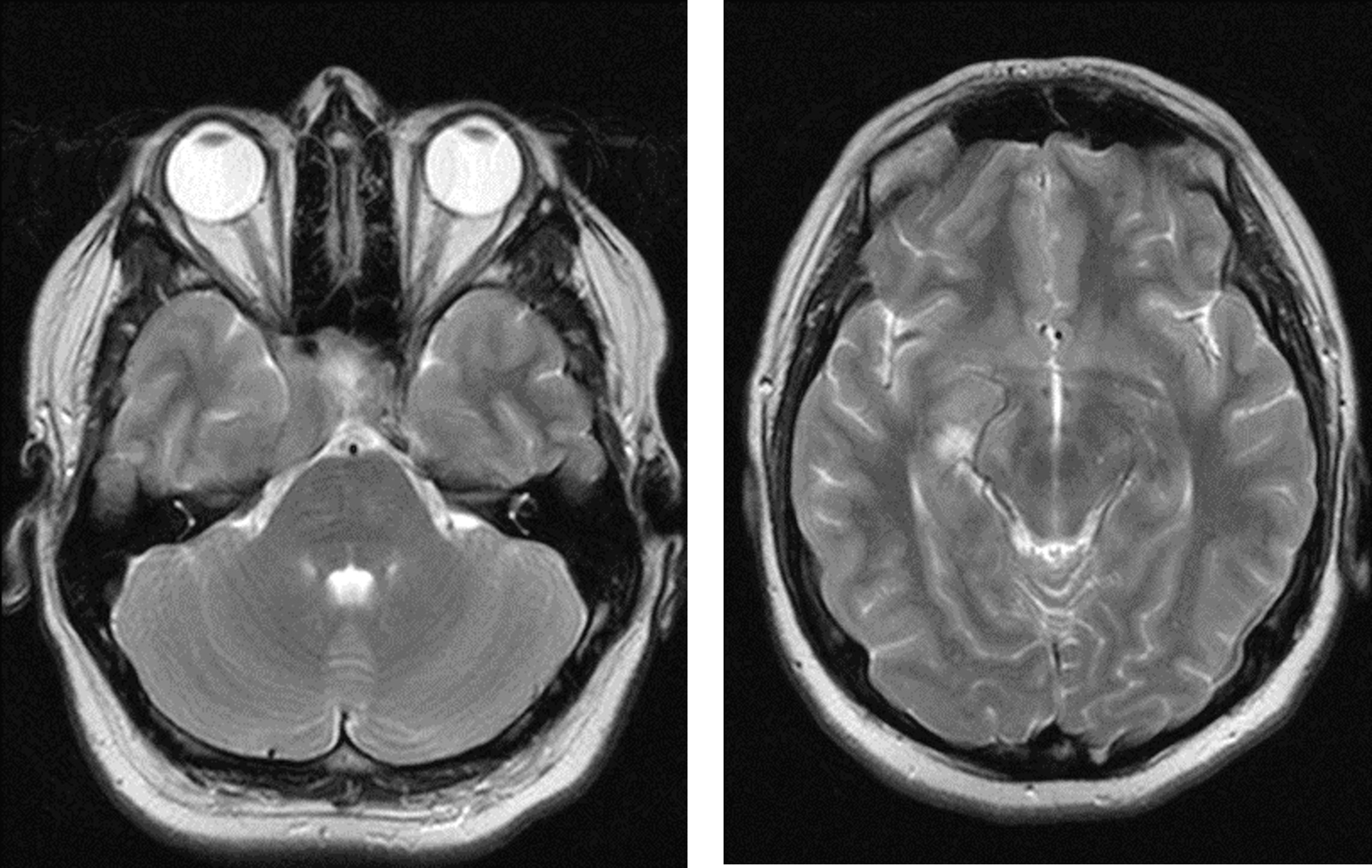
Case Presentation: A 32 year old male presented with worsening headaches over several weeks. He had multiple previous visits to medical and psychiatric facilities often leaving against medical advice (AMA). On his last hospital visit, a large brain mass was discovered on imaging. However, he left AMA before work-up was complete. He was later brought to the emergency department by family with concerns that he had not been himself for several months and exhibited worsening impulsive and erratic behavior. He was unable to perform his job as a mechanic, had crashed his car multiple times, was involved in several altercations and had a gun pulled on him for walking into unknown homes. On admission, the patient was minimally cooperative. Physical exam revealed slight right eye ptosis with no other neurological deficits. Labs were unremarkable with the exception of prolactin level >10,000, TSH 1.49, FT4 0.6 and testosterone 33. The toxicology screen was positive for cannabinoids. CT and MRI imaging of the head showed a large (54.4mm x 34.5mm) sellar/suprasellar mass with superior extension resulting in mass effect, compression of the 3rd ventricle and early obstructive hydrocephalus. During his work-up, the patient became anxious and wanted to leave AMA. He was rambling, restless and impulsive and deemed to be a danger to himself and others. He was placed on a medical hold and later found to be non-decisional by Psychiatry. He was also evaluated by Neurosurgery, Ophthalmology and Endocrine. Surgical intervention was not warranted and medical management was initiated with high dose steroids, cabergoline, levothyroxine, quetiapine and valproic acid. Throughout his hospitalization, he continued to display impulsive and dangerous behavior, threatening to leave and attempting to do so. This led to a prolonged hospitalization as the team could not ensure a safe and appropriate discharge. After a few weeks of treatment, his behavior, judgement and insight improved enabling a safe discharge home. After 3 months of treatment, his tumor size decreased, hydrocephalus resolved, prolactin and testosterone levels nearly normalized and symptoms improved.
Discussion: While prolactinoma is the most common pituitary adenoma in adults, giant prolactinoma is relatively rare. It accounts for 1-5% of prolactinomas and is defined by size >40mm in diameter. Typical presentation includes headache, vision changes and amenorrhea in women and hypogonadism and erectile dysfunction in men.
Conclusions: There are few reports of giant prolactinoma presenting with behavioral or psychiatric symptoms. This case seeks to add to the current body of literature and to inform Hospitalists of this unusual presentation of a rarely occurring pituitary tumor. It also highlights the unique safety challenges that may accompany this condition and emphasizes the need for early safety interventions and a collaborative approach to care.