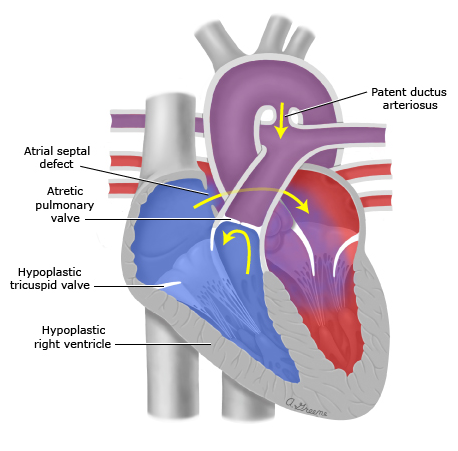
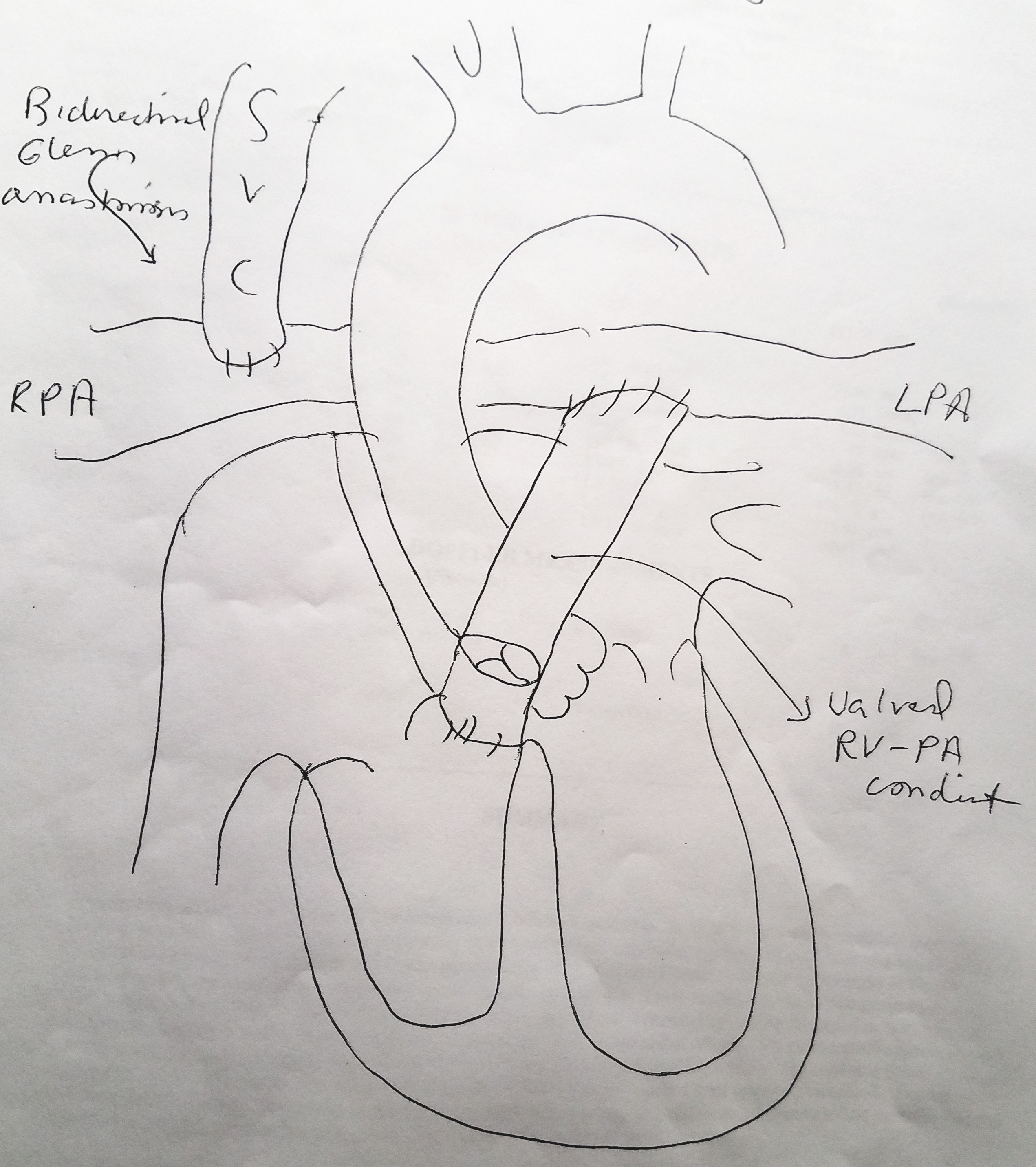
Case Presentation: We present a 20 year old gentleman in acute hypoxic and hypercapnic respiratory failure and cariogenic shock secondary to hemodynamically unstable hemoptysis requiring mechanical ventilation and vasopressor support with norepinephrine and vasopressin. He had history of pulmonary atresia with intact interventricular septum at birth post right ventricular outflow repair and 1.5 ventricular repair (Bidirectional Glenn anastomosis). Emergent bronchoscopy was performed which localized the source of bleed to the right lower lobe. Hemostasis was obtained following IR guided arteriogram and embolization of Right bronchial, T1-T4 intercostal and Right internal mammary arteries. Patient’s hemodynamics and oxygenation were difficult to maintain even after paralysis, high FiO2, and sufficient PEEP. Acute hypoxic cardiac arrest occurred 24 hours post embolization, with successful ROSC after 2 minutes. A decision was made to (1) substitute Norepinephrine and Vasopressin for Epinephrine and Milrinone, (2) the addition of inhaled Nitric oxide to improve V/Q mismatch and (3) lower PEEP for increased venous return. With these changes, notable improvement was noted in his hemodynamics and oxygenation. Slowly these support modalities were weaned down, and patient was extubated 5 days later with complete recovery to baseline and discharge 4 days after.
Discussion: Vasopressor/Inotrope management:Norepinephrine is considered the vasopressor agent of choice in cardiogenic shock. However, in patients with 1.5 (hybrid) Glenn physiology the goal is to increase pulmonary flow and thus systemic flow. This is best realized with the use of Epinephrine and Milrinone. The use of Milrinone allows for lower Systemic Vascular Resistance, lower Pulmonary Vascular Resistance, and further contributes to the lusitropy/ Ionotrophy offered by epinephrine. This combination lead to the ideal perfusion status in this patient.
Oxygenation:
As the Superior Vena Cava drains directly into the right pulmonary artery in patients with Glenn bidirectional physiology, it is important to note that forward flow depends heavily on preload. To oxygenate by increasing PEEP, we compromise venous return and pulmonary blood flow. Therefore, with introduction of inhaled nitric oxide in combination with epinephrine and milrinone we promoted intrapulmonary arteriolar dilation, oxygenation and improve V/Q mismatch.
Conclusions: Although rare, physicians should be aware of unconventional treatment modalities for patients with Glenn physiology since early appropriate intervention is imperative for survival.