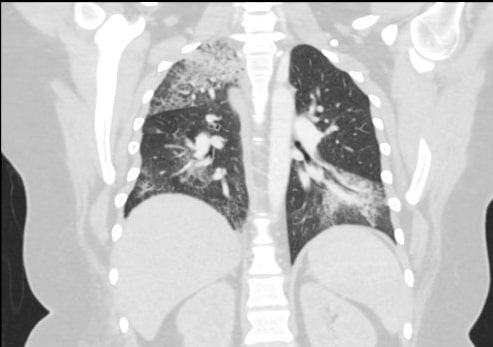
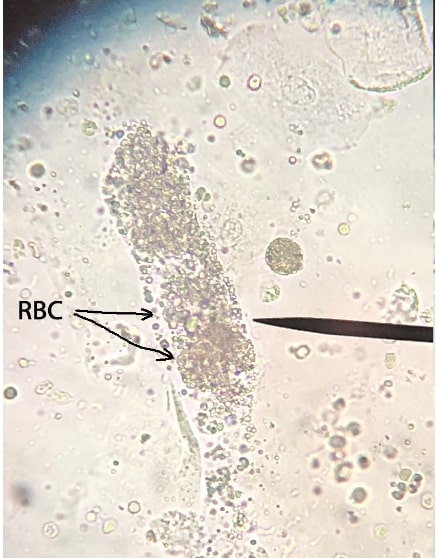
Case Presentation: Goodpasture’s disease is an autoimmune condition characterized by pulmonary hemorrhage, glomerulonephritis and production of anti-GBM (glomerular basement membrane) antibodies. Anti-GBM disease approximately accounts for 15 percent of all cases of crescentic glomerulonephritis. We report a young female patient diagnosed with Goodpasture’s disease who initially presented with recurrent pneumonias.A 19 year old female patient presented to the hospital with 1 week of progressive dyspnea, cough, hemoptysis (2 teaspoonfuls) and fatigue. These symptoms originally started 2 months prior to her initial presentation which resulted in a couple of ER visits and a hospitalization where she was treated with antibiotics for a presumed pneumonia during all of the visits. Her past medical history is significant for well-controlled mild intermittent asthma, allergic rhinitis, morbid obesity and GERD. On admission, the patient was tachypneic and hypoxic requiring high flow oxygen, wheezes on lung auscultation and an otherwise normal physical examination. Chest X-ray showed bilateral infiltrates; computed tomography of the chest was negative for pulmonary embolism and urinalysis was positive for red cell casts and a urine protein/creatinine ratio of 1.46, suggesting significant proteinuria. Laboratory results also revealed acute kidney injury with a creatinine of 1.23. Complete blood count was normal with no evidence of eosinophilia. The anti-GBM antibody was elevated at 36U (normal range is < 20U), and other autoimmune workup was negative (ANCA , MPO, PR3, ANA with normal C3 and C4 levels). Renal biopsy showed crescentic glomerulonephritis (18 out of 24 glomerulus involved ), all these findings were consistent with Goodpasture’s disease. Based on this, the patient was immediately started on steroids, cyclophosphamide and completed 5 rounds of plasmapheresis. Her symptoms improved drastically and was discharged home safely on a tapering steroid dose and cyclophosphamide.
Discussion: Majority of patients with anti-GBM disease present only with clinical features of rapidly progressive glomerulonephritis (RPGN) and /or concomitant alveolar hemorrhage. Usually a very small proportion of patients may present with isolated pulmonary findings which is similar to our patient as she initially presented with isolated recurrent pneumonias, followed by subsequent development of RPGN later on (1). Laboratory findings often include: anemia, microhematuria, proteinuria, increased levels of urea and creatinine and anti-GBM antibodies. Diagnosis of this syndrome can be established by the presence of pulmonary hemorrhage, chest radiography findings, kidney biopsy and positive result of circulating anti-GBM antibodies. Treatment should be initiated as soon as possible using a combination of corticosteroids, cytotoxic medications and plasmapheresis. A combination of these therapies have proven a promising benefit.
Conclusions: Physicians taking care of young patients presenting with recurrent pneumonias, should have a high index of suspicion for vasculitis, especially Goodpasture’s syndrome, as a delay in the management can be harmful to the patient.